Flipping the newspapers or news sources over the internet, it is evident that the rising chronic conditions in the aging population will burden healthcare providers. According to the American Hospital Association, around 133 million people in the United States suffer from at least one chronic disease. Moreover, the lifestyles the current generation lives in will further give rise to people suffering from multiple chronic conditions.
The impact it can have on the economy and other aspects of growth and life expectancy. To overcome this, the Centers for Medicare and Medicaid Services (CMS) introduced a Remote Patient Monitoring program to reduce the burden on healthcare providers and enhance technology with the use of technology.
But how do you secure the reimbursements?
Understanding RPM Reimbursement Landscape
Remote patient monitoring programs offer great opportunities to gain maximum reimbursement. However, to achieve that, understanding the reimbursement landscape is essential. Though many healthcare providers find it difficult to comfortably navigate through the landscape, if you know the right way, it becomes significantly easier. Let’s discuss this in brief to understand better:
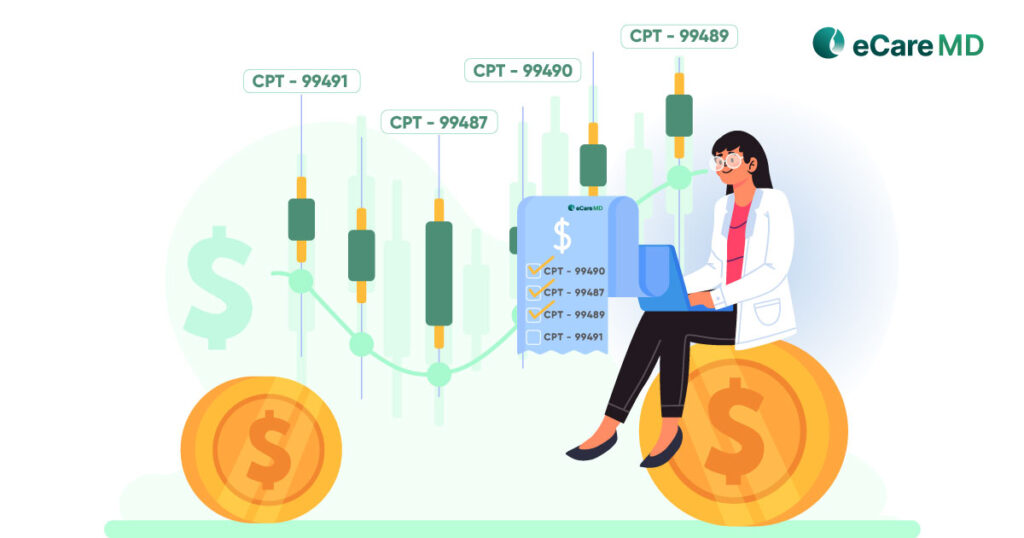
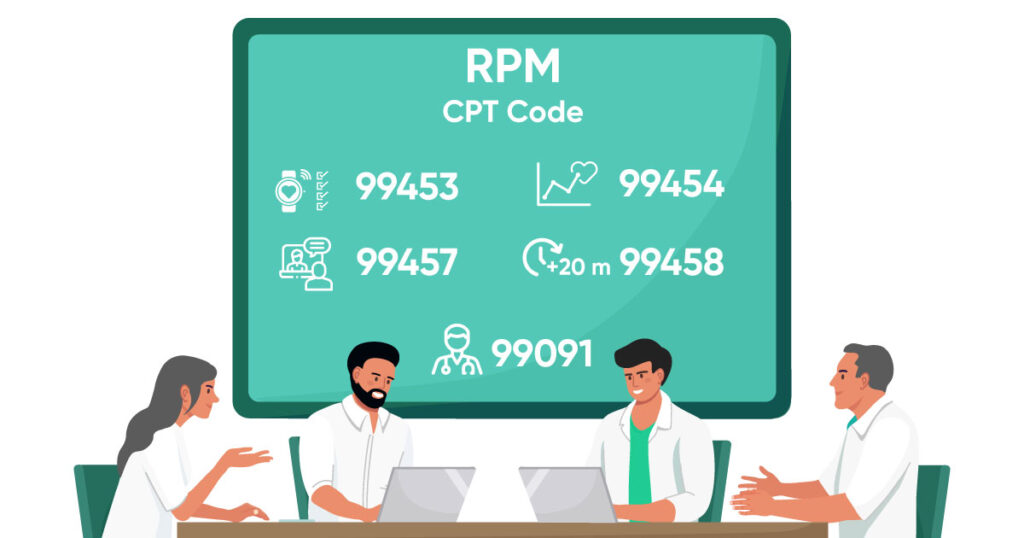
1. Medicare Guidelines & CPT Codes
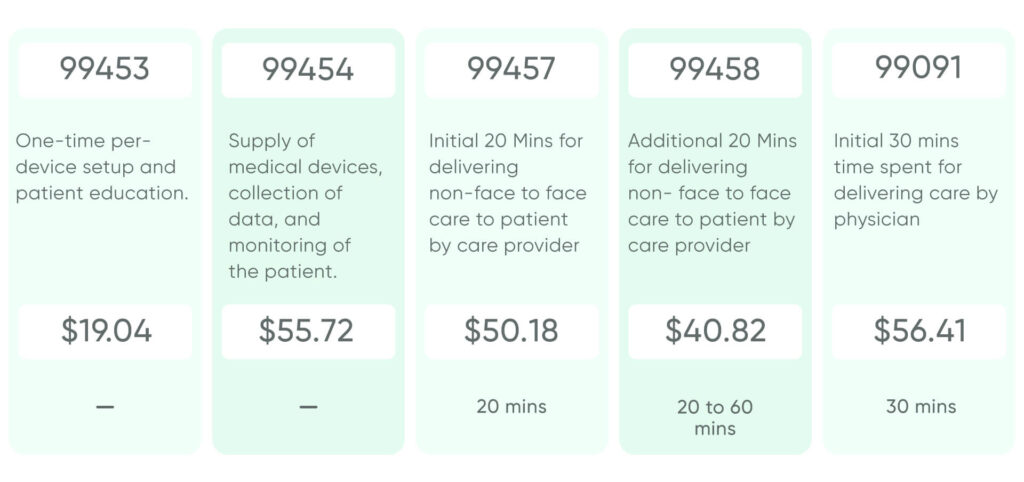
The Center for Medicare and Medicaid Services (CMS), to bring ease to the billing, insurance claims, and reimbursement process, has assigned some specific Current Procedural Terminology Codes or CPT codes for Remote Patient Monitoring services.
- CPT Code 99453: The code refers to the initial set-up, patient education, and equipment cost that the provider provides to the patient. This is a one-time fee that the provider cannot bill every month. The national average for this code is $19.04.
- CPT Code 99454: This code refers to the supply of remote patient monitoring devices to the patient. To qualify for this code, the provider should supply the RPM devices, collect patient vitals for at least 16 days, and report the summary of services to the clinician. The national average for this code is $55.72.
- CPT Code 99457: This code refers to remote physiologic monitoring services provided by a care provider for a total of minimum 20 minutes over a period of 30-days. The national average for this code is $50.18.
- CPT Code 99458: This code is an add-on code to CPT Code 99457 for remote physiologic monitoring by clinical staff for an additional cumulative 20 minutes of RPM services over the period of 30 days. The national average for this code is $40.82.
- CPT Code 99091: This code refers to the collection and interpretation of data by a physician for a cumulative 30 minutes over a period of 30 days. The national average for this code is $56.41.
2. Commercial Payer Coverage
Free Guide - Key Considerations for Different Commercial Payers for CPT Codes for RPM services
Download now3. Staying Updated with the Regulations
Optimizing Your RPM Billing Process
1. Accurate Documentation & Coding
2. Patient Selection & Eligibility Verification
3. Streamlined Workflow & Claim Submission
Strategies for Maximizing Reimbursement Success

1. Proactive Communication with Payers
2. Appealing Denied Claims
3. Ongoing Program Evaluation & Improvement
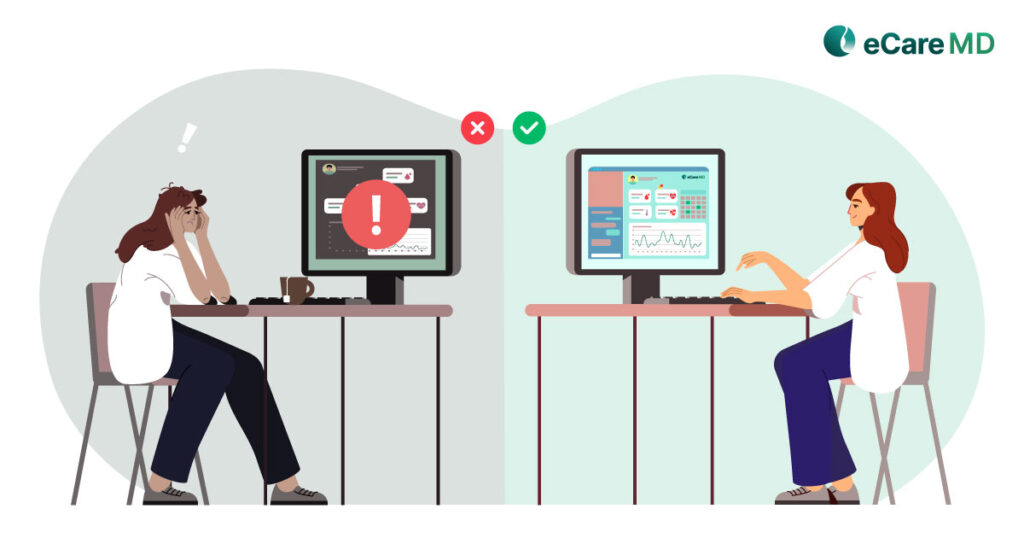
Minimizing Claim Denials & Maximizing Revenue
1. Understanding Common Denial Reasons
The first step to minimize claim denials is to understand the most common reasons for denial in your practice. This would usually include incorrect coding, missing documents, or patient ineligibility to quality for the RPM program. Here, the remote patient monitoring software can come in handy to help you identify patterns and trends and take appropriate measures to overcome them.
2. Appealing Denied Claims
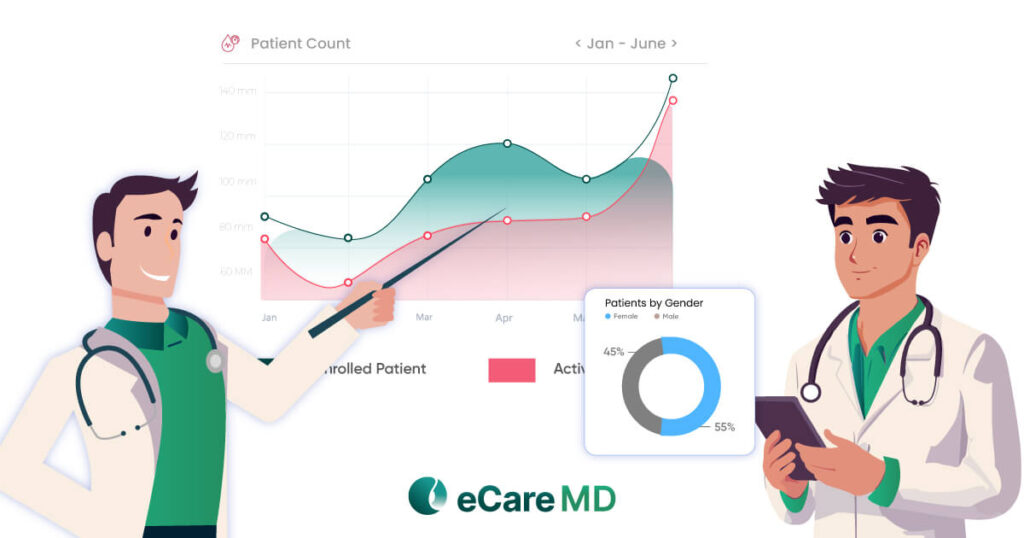
3. Performance Tracking & Analytics
The most important part is tracking and analyzing the entire billing cycle and process. Set some key performance indicators for your process, like claims submission rates, to check efficiency and denial ratio to identify the areas for improvement and optimize your program and procedure accordingly for maximum program profitability.
Conclusion
Optimizing reimbursement simply means maximizing reimbursements from the CMS RPM Program. And the best way to do that is to follow the best practices mentioned above and curate your workflow accordingly. However, the major part of it lies with compliance and patient education, which can help you make the most out of the RPM program.
However, since the healthcare industry is evolving from reactive to proactive, you, as a provider, need to take proactive measures to ensure the financial success of RPM initiatives. This will help you enhance and expand your healthcare practices and drive positive patient health outcomes.
Frequently Asked Question’s
The CMS Remote Patient Monitoring (RPM) program allows Medicare providers to get reimbursed for monitoring patients’ health data remotely. This data can include weight, blood pressure, and blood sugar.
By using approved devices and following specific guidelines, healthcare providers can earn money for keeping tabs on patients outside the office. This can improve patient care and potentially reduce hospital visits, saving the healthcare system money.
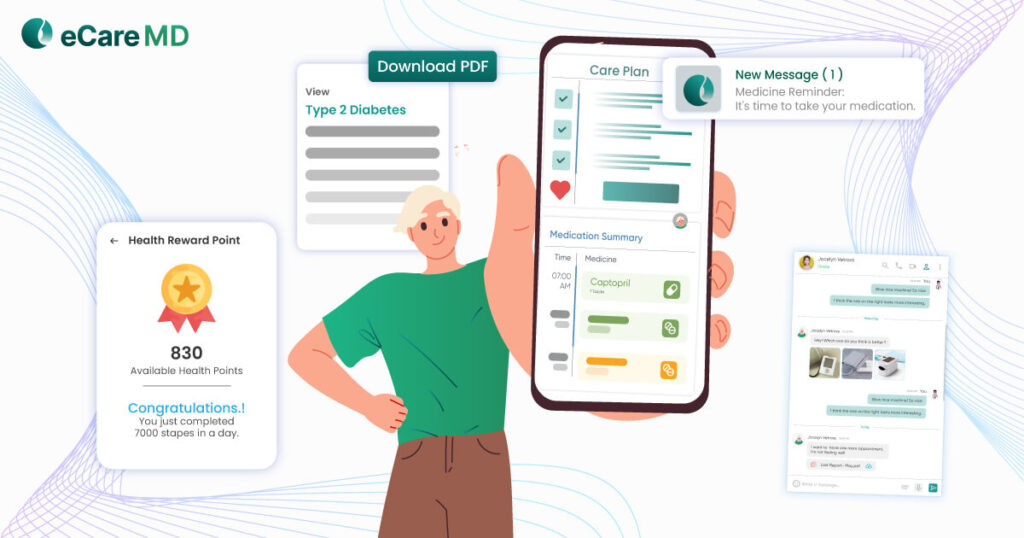
- Streamlining data collection: Automated tools can gather patient vitals and health info from wearables and devices, reducing manual entry and errors.
- Enhancing remote monitoring: Software can provide clinicians with real-time patient data dashboards, allowing for quicker interventions and adjustments to care plans.
- Improving patient engagement: Mobile apps and secure messaging features can empower patients to actively participate in their care, improving adherence and overall health outcomes.
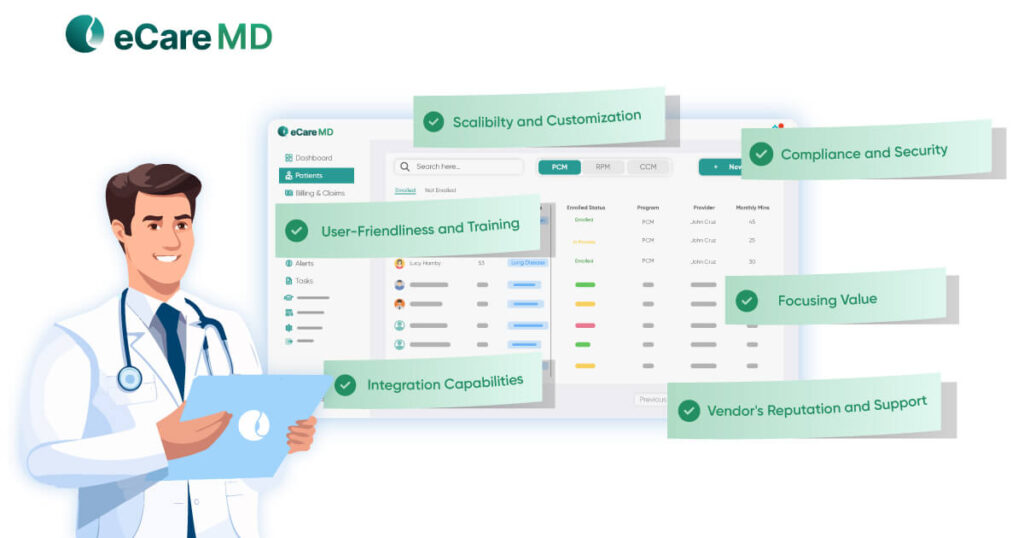
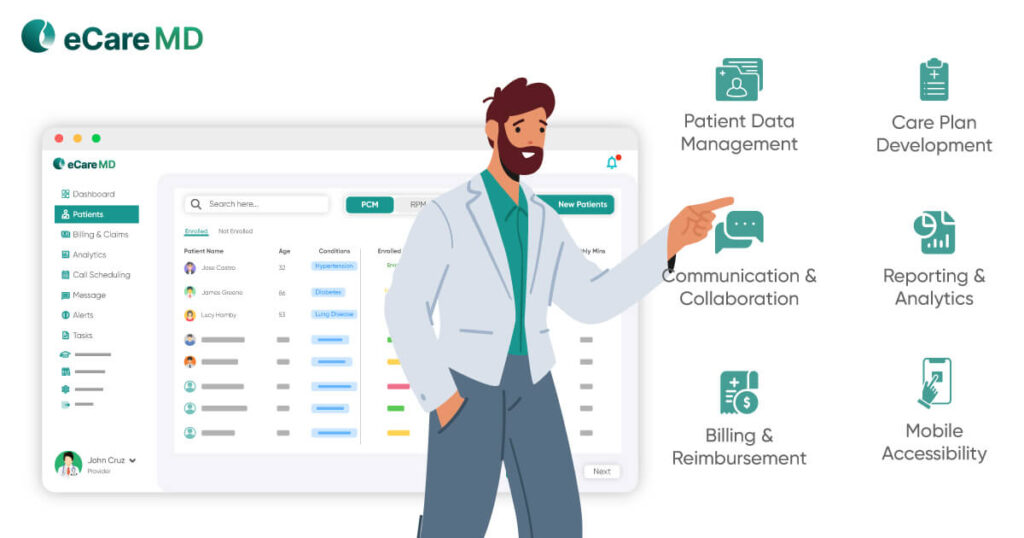
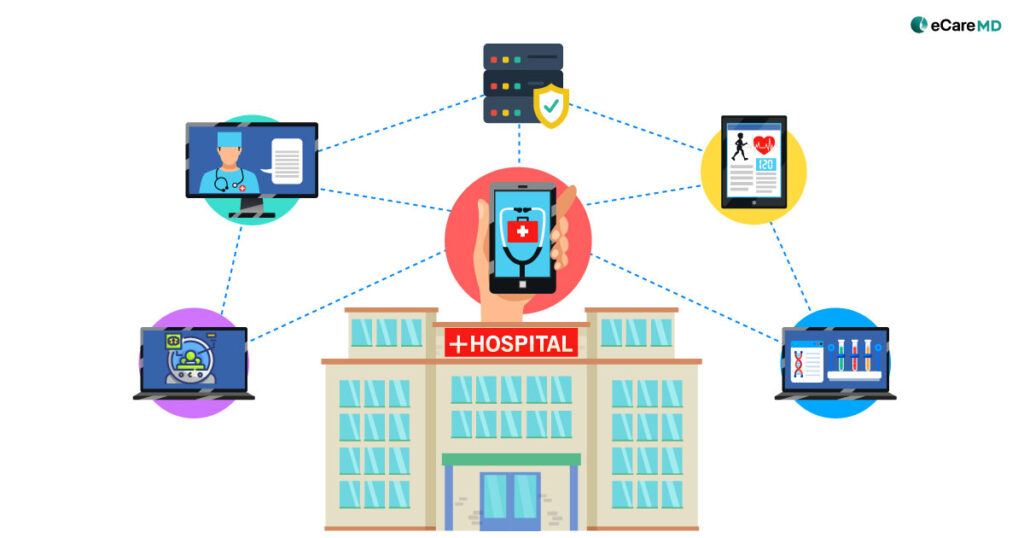
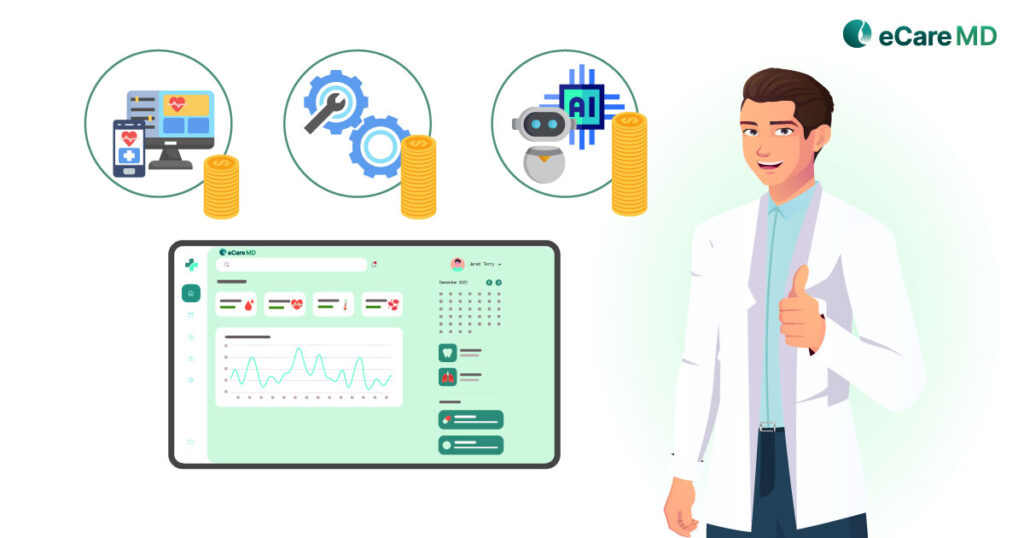
Here are key factors for healthcare providers choosing RPM software:
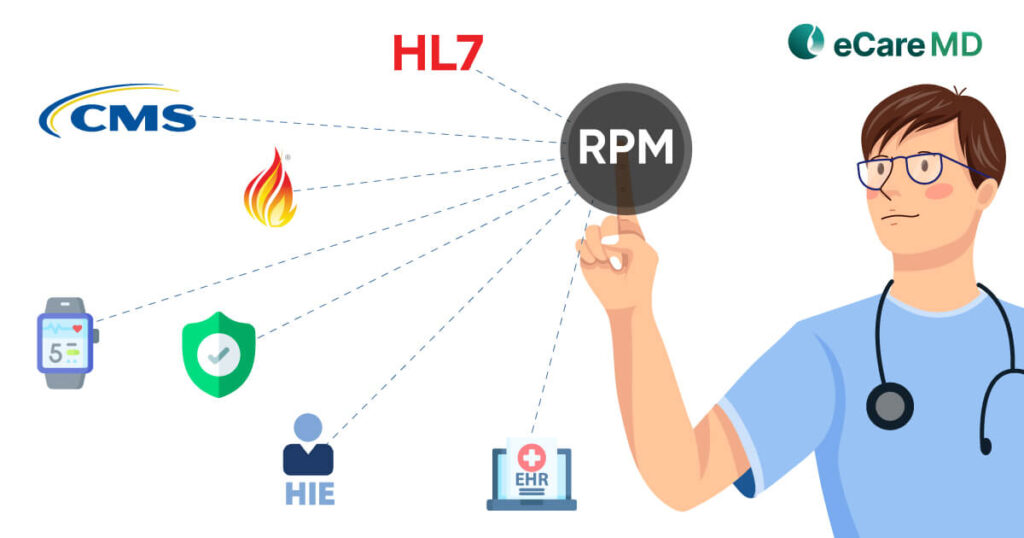
- Compatibility: Ensure it integrates with your existing Electronic Health Records (EHR) system to avoid data silos.
- Data Security: HIPAA compliance is crucial for protecting patient privacy.
- Ease of Use: Staff should find it user-friendly to minimize training time and ensure efficient workflow.
- Device Integration: Confirm compatibility with your chosen RPM devices for seamless data collection.
- Reporting & Analytics: Robust reporting tools help track patient progress and program effectiveness.
Consider your budget and program size as well. Aim for software that scales with your needs.
Healthcare organizations implementing CMS RPM programs face hurdles in three main areas:
- Behavioral: Patients and staff with limited tech knowledge or concerns about the program’s effectiveness can be resistant to adopting new devices and workflows.
- Organizational: Integrating RPM into existing workflows, training staff, and coping with potential staff shortages can disrupt smooth implementation.
- Financial: Start-up costs for equipment and potential revenue model uncertainties can be a concern for healthcare organizations.
To boost engagement with RPM programs:
- Focus on patient needs.
- Start by understanding your audience and tailor enrollment accordingly.
- Provide clear explanations of program benefits and ensure user-friendly devices.
- Educate patients throughout the process and offer ongoing support.
- Leverage technology for reminders, progress tracking, and easy communication.
- Spot trends and issues early: Catching problems before they escalate can prevent costly ER visits and hospitalizations.
- Tailor treatment plans: Data helps adjust medications and therapies for better individual results.
- Boost patient engagement: Patients see their progress and are empowered to manage their health.
- 99453: Initial setup (e.g., explaining device use). Billed once per episode.
- 99454: Monthly monitoring, device supply, and servicing. Requires at least 16 days of data collection.
- 99457: Non-face-to-face care (20 minutes/month). It can be used with add-on codes for additional time.
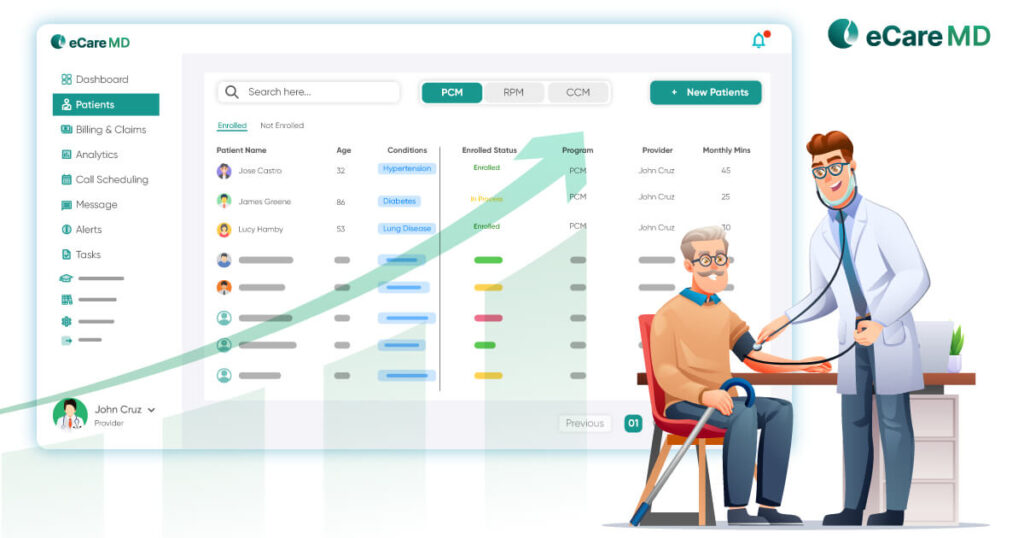
- Target high-risk patients for efficient chronic disease management.
- Leverage software to automate tasks and optimize workflows.
- Focus on preventative care to reduce readmissions and improve patient outcomes.