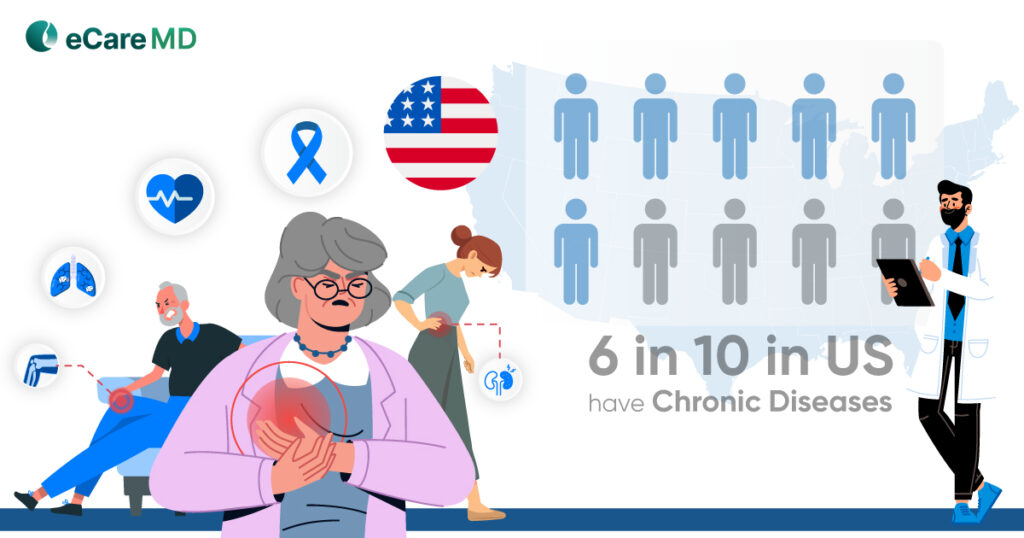
If you closely observe your practice database about hospital readmission, chronic patients would be leading the charts with the highest number of hospital readmissions. Statistically, chronic patients make up around 81% of the hospital readmission.
The number of patients with chronic conditions has risen drastically over the last few decades. To further worsen the situation, the changing lifestyles in the currently aging population, the global burden of chronic diseases is predicted to increase by 56%, according to the United Nations.
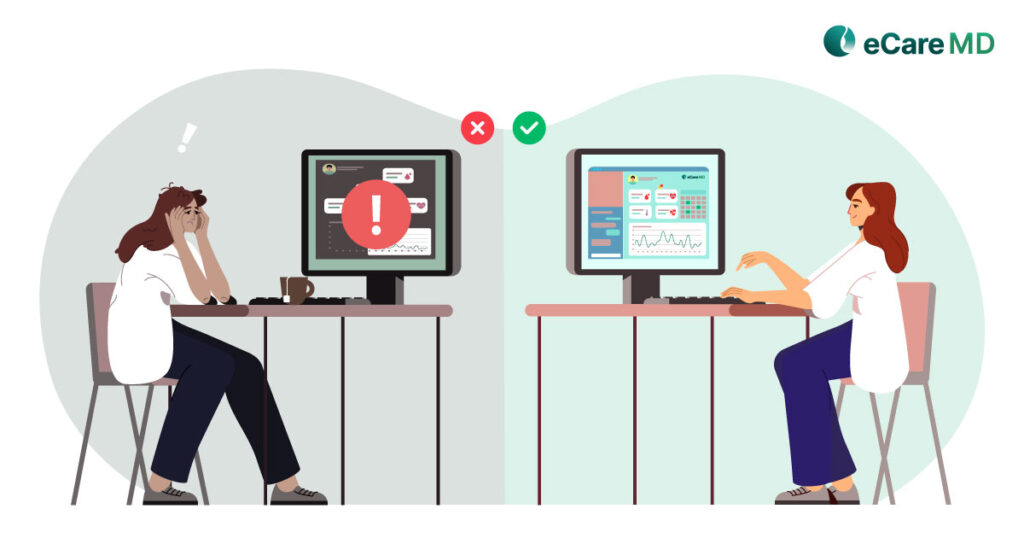
And it’s not a secret that chronic conditions require highly specialized, attentive, and continuous care. The rise in chronic conditions has disrupted the healthcare system. While most healthcare professionals like yourself spend most of their time treating chronically ill patients, the care services for others appear to be lacking.
To bring the focus back to treating patients who are in need, the Centers for Medicare and Medicaid Services (CMS) in 2015 started the Chronic Care Management Program. It not only shifted the focus to better patient-centric treatment but also eliminated the time-delay factor while providing care services.
As it creates a win-win situation for your practice and patients, wouldn’t it be logical to start your own CMS CCM program?
In this blog, we’ll give you 5 reasons why you should start your own CCM Program and a 7-step implementation guide to make it easier.
So, without further ado, let’s get started!
5 Reasons Why to Start the CCM Program
Features define the functionality of any program, which gives you benefits or reasons to start the program yourself. So, here are the five reasons why you should start your own chronic care management program:
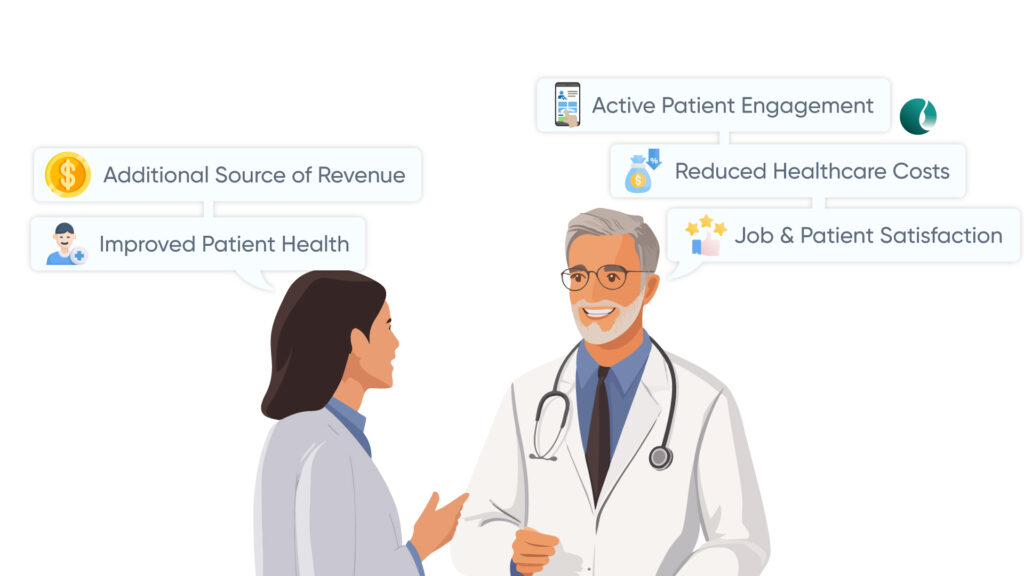
Reason 1: Additional Source of Revenue:
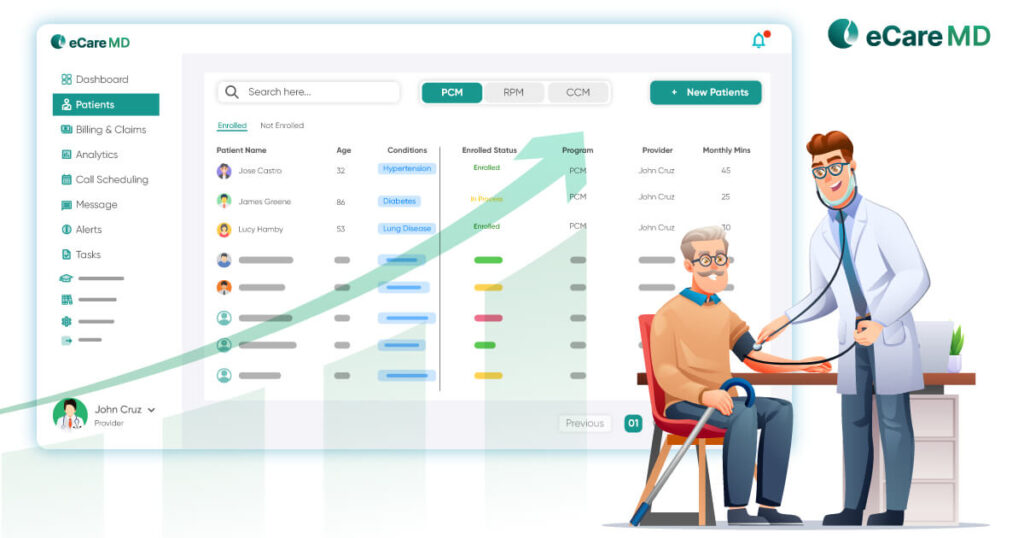
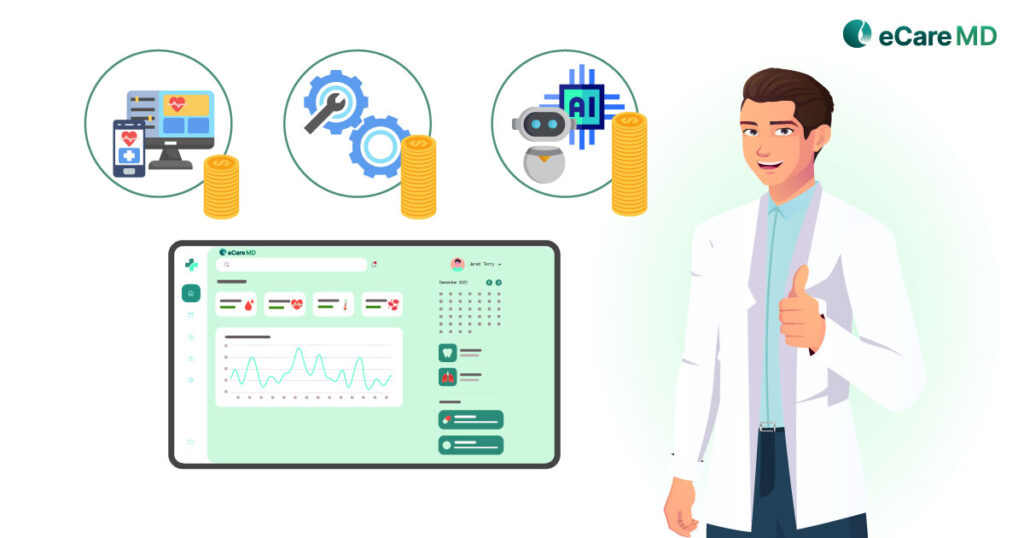
Medicare and other federal and private insurers provide reimbursement programs for your chronic care management program. This acts as an additional source of revenue apart from your healthcare practice and offsets the cost of care for your patient population with chronic conditions.
Reason 2: Improved Patient Outcomes:
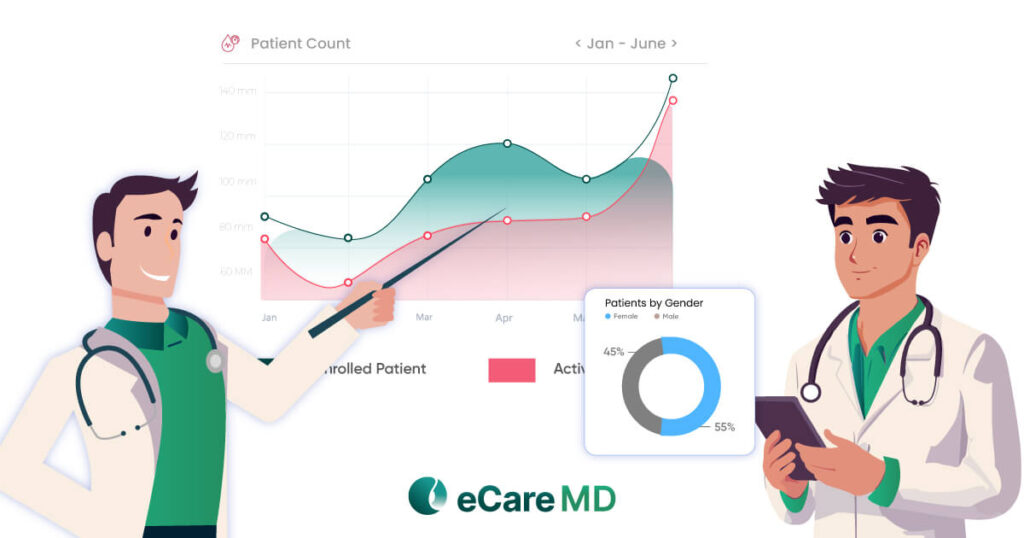
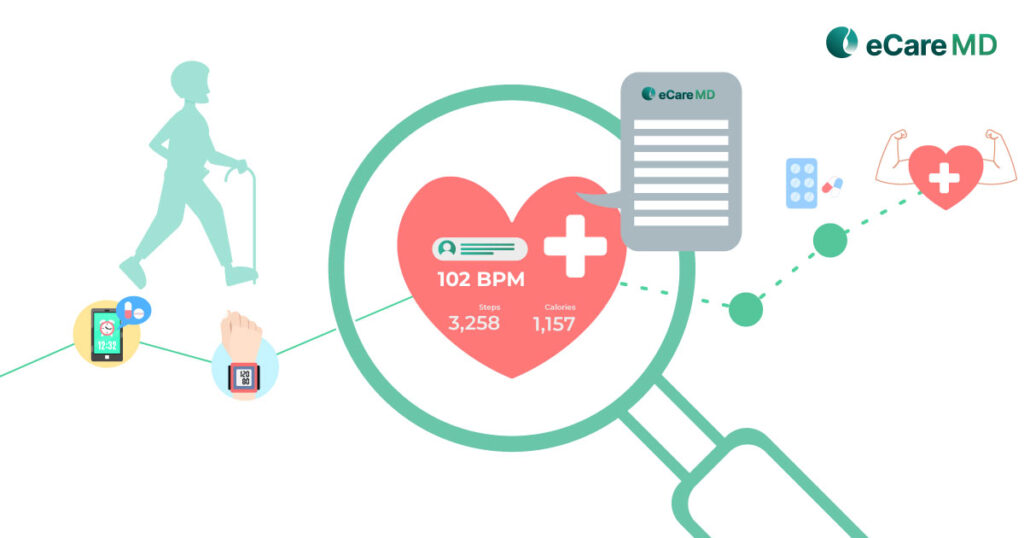
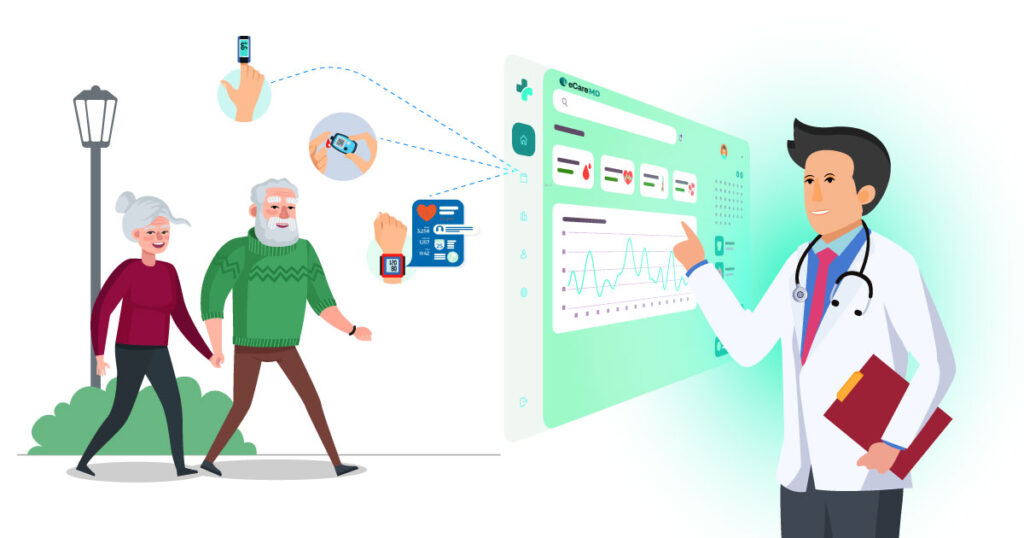
A chronic care management program with the help of RPM allows you to provide ongoing support and guidance to the patient regarding their health. This way, you and the patient can enhance disease control, reduce symptom severity, and avoid complications. This directly or indirectly contributes to significantly improving patient outcomes. Some of the studies showing improved health outcomes in chronic conditions are diabetes, hypertension, obesity, and chronic lung diseases.
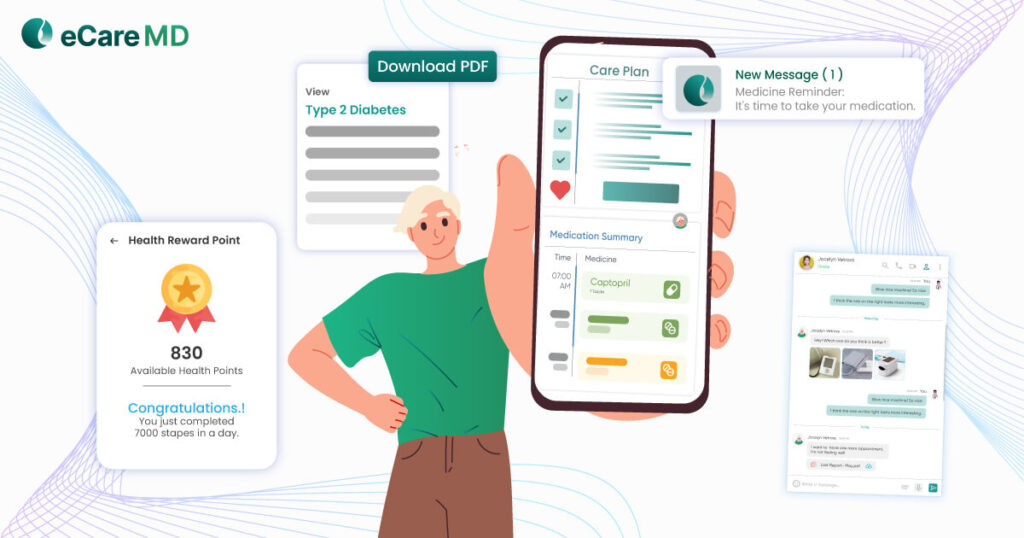
Reason 3: Better Patient Engagement:
Chronic care management imbibes data-driven, patient-centric care practices. This increases collaboration and gives your patient more control of their health. Regular communication, creating personalized care plans, and making informed decisions not only keep the patient engaged with their care activities but also play an active role in proactively managing their health. Since the patient is engaged with their care activities, it increases medication adherence and results in fewer hospital visits, allowing you to utilize your healthcare resources optimally.
Reason 4: Reduced Healthcare Costs:
Reason 5: Job and Patient Satisfaction:
7-Step Implementation Guide
The features and benefits of a chronic care management program are quite lucrative, aren’t they?
Well, they indeed are, but its implementation process can be quite complicated if you don’t know the way around. Simplifying the process, here is a seven-step easy CCM implementation guide for you.
Or
Click here to watch the ‘How to Successfully Implement CCM Program’ webinar.
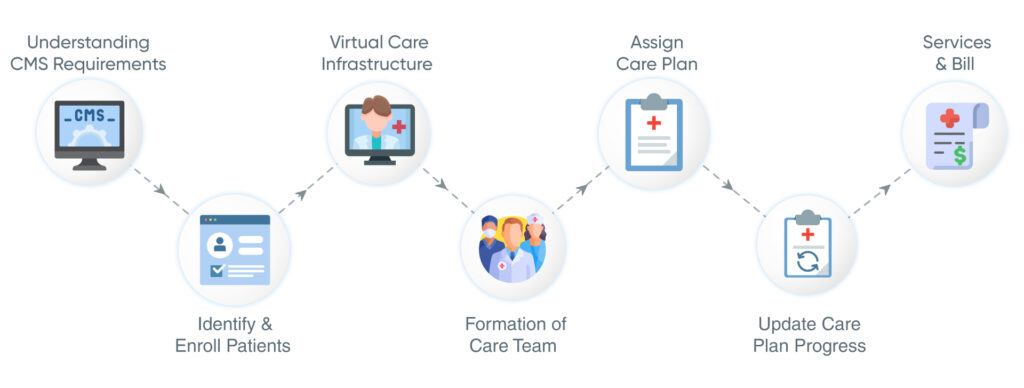
Step 1 - Understanding CMS Requirements
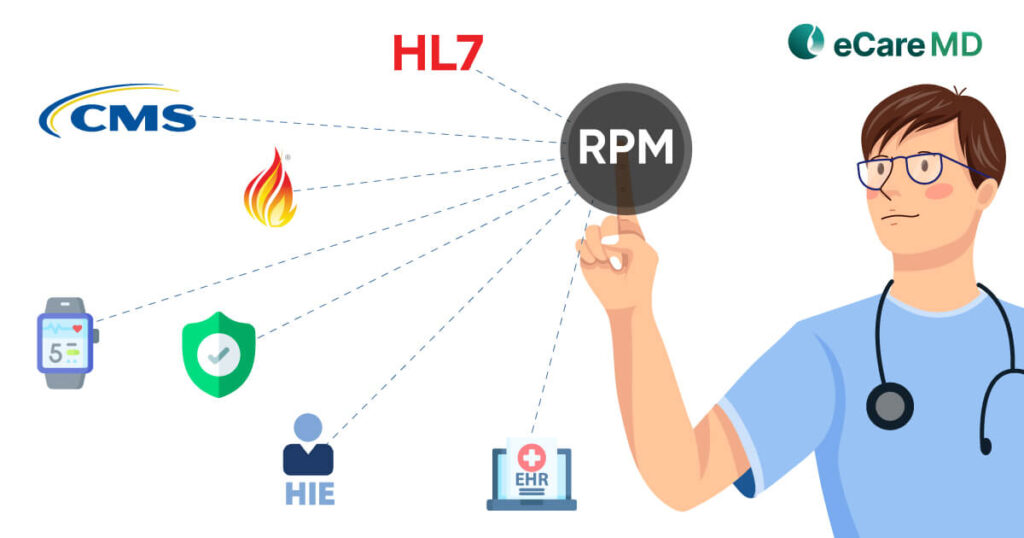
Before kickstarting your own CCM program, it is important for you to understand program requirements set by the Centers for Medicare and Medicaid Services (CMS). CMS has set clear and specific guidelines for the initiation of a chronic care management program. These guidelines include patient eligibility criteria, documentation, billing codes, and reimbursement regulations. It is important for you to adhere to the guidelines to avoid any legal complications and maximize your reimbursement. Read the CMS CCM program guidelines here.
Step 2 - Identify and Enroll Patients
Step 3 - Set up Virtual Care Infrastructure, Invite & Enroll Patients
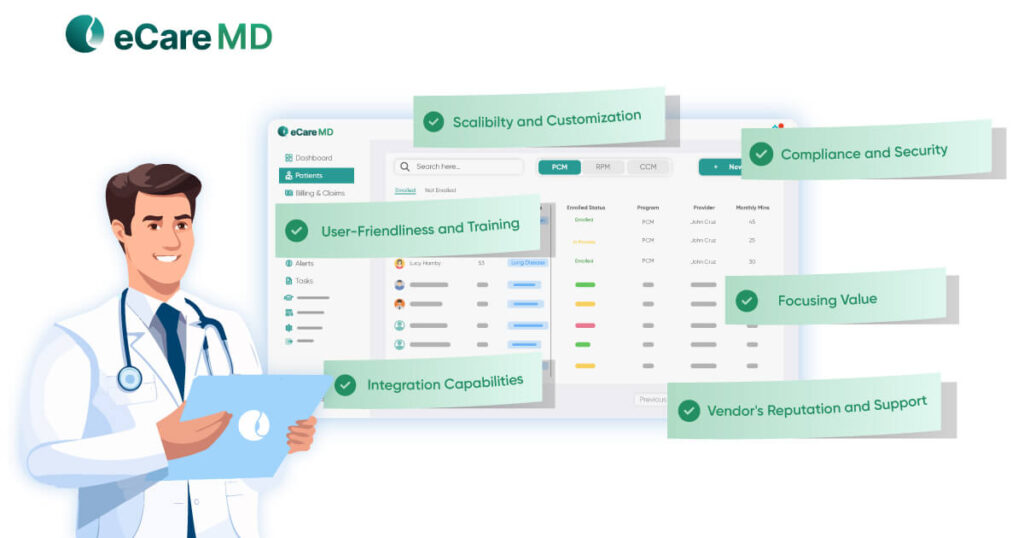
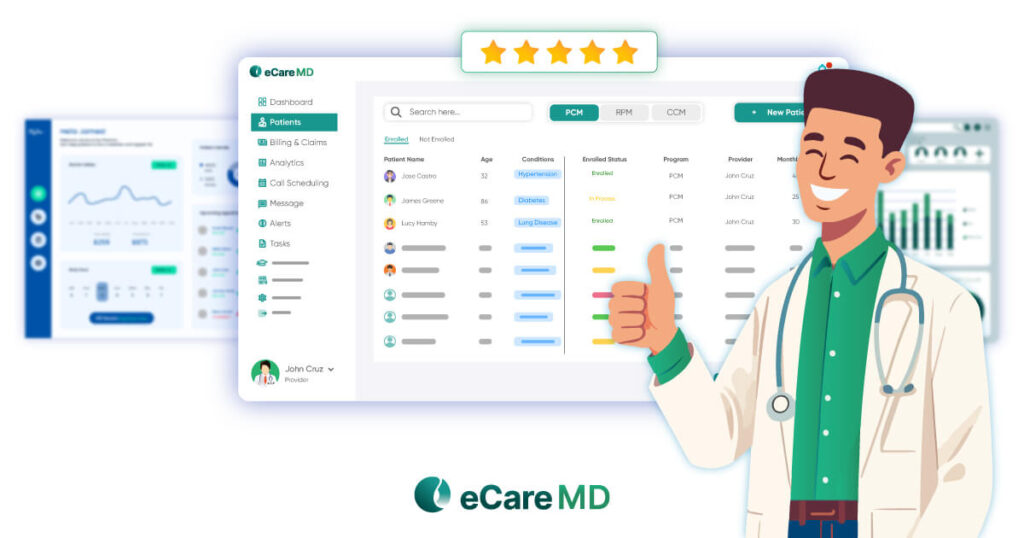
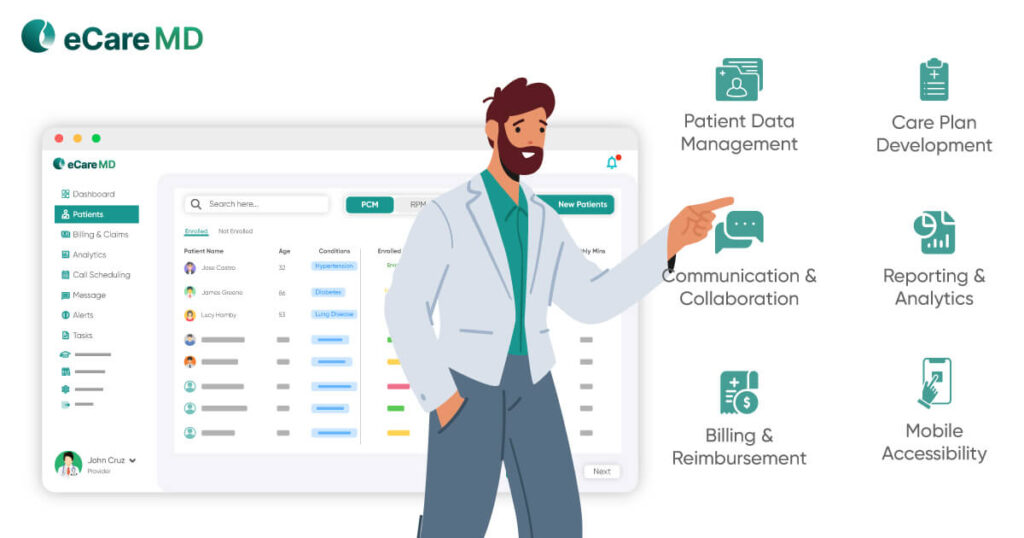
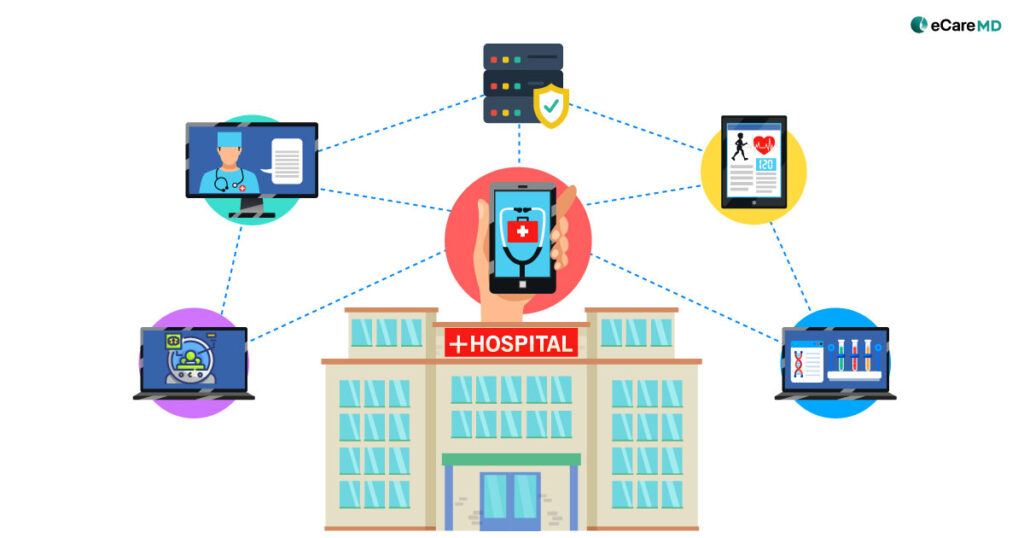
Since the CCM program will digitize your healthcare practice, you need to set up a secure virtual care infrastructure to enable virtual care delivery. This will need a Chronic Care Software that will align perfectly with your practice’s workflow and have all the essential features required for providing care services. The software for chronic care management should have features like analytics and reporting, customization and integration, user-friendly UI/UX, and ongoing vendor support and maintenance. Along with that, you will also need to set up RPM devices to enable remote monitoring.
While developing the virtual care infrastructure, special emphasis should be given to making the ecosystem secure since it will majorly deal with sensitive patient information. That is why we chose the vendor carefully to implement the program successfully. Also, after the setup of virtual care infrastructure, then, starts inviting patients to get enrolled in CCM program by sending them consent forms and enrolling the patients who have given their consents.
Step 4 - Training & Formation of Care Team
To run the chronic care management program, you need to build a multidisciplinary care team for the delivery of care to the patients enrolled in your CCM program. Your care team should include qualified healthcare professionals, which usually include physicians, clinical nurse specialists, care managers, and others with specialists with respect to your patient population.
What is the point of starting a CCM program when your healthcare staff does not know how to deliver and bill for the services you are providing? That is why crucial attention should be paid to the training process. Effective hands-on training with the chronic care management solution and other aspects of the program can help them understand the workflow better and increase the CCM program’s acceptance rate.
Step 5 - Assign Care Plan
Step 6 - Monitor, review, and update patient care plan progress
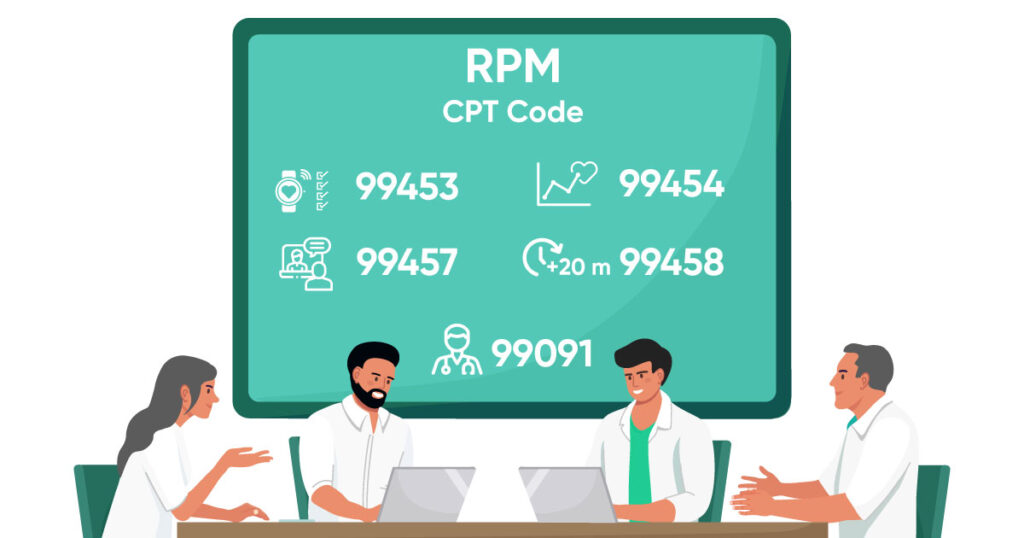
Step 7 - Log time for services and Bill
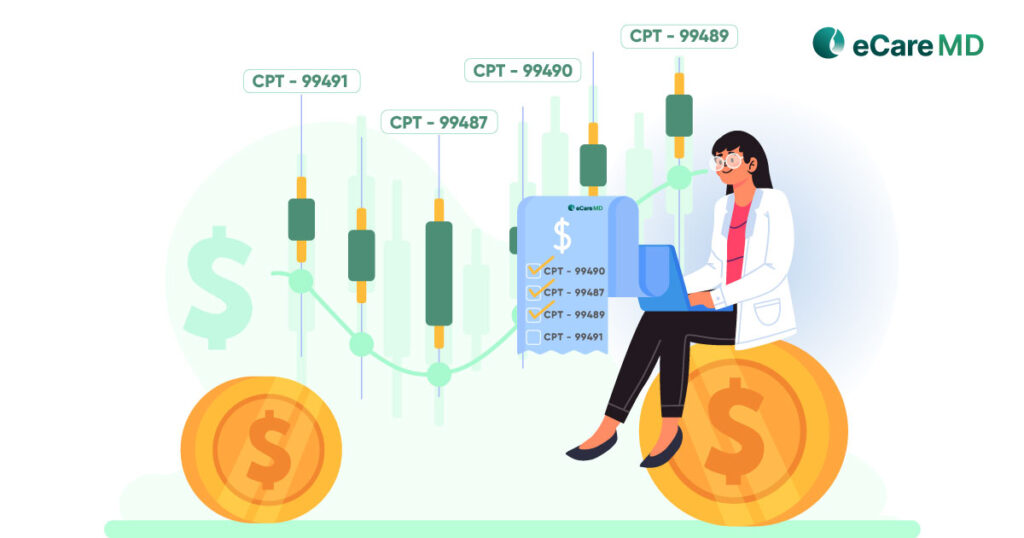
Once you’ve checked all the above steps, it is time to log the time for providing care services to the patients enrolled in your program. After each service, it is important for you to bill for the services you have provided.
To suit a claim through CMS, here are the five check-box you need to tick:
- CPT Codes for each program you are managing.
- ICD-10 codes specific to the conditions you are managing.
- Date of Service
- Place and Mode of Service
- National Provider Identifier Number (NPI).
Along with this, here are four steps to bill for chronic care management services:
- Cross-check and verify the CMS requirements for each patient every month
- File the claims with CMS monthly
- Send an invoice to the patients every month for the CCM services provided
- Ensure that there are no conflicting codes to eliminate the chances of claim denials.
Conclusion
With the digitization of healthcare practices and the rising number of chronically ill patients, the chronic care management program is going to play a crucial role in the future of healthcare. While still in the transition process, it is important to know its distinct features, benefits, and the implementation process for its success. Let this blog be your guide to the program’s successful implementation.
Frequently Asked Question’s
CMS CCM covers beneficiaries with two or more chronic conditions expected to last at least 12 months. Specific conditions aren’t listed, but examples include diabetes, heart disease, and chronic obstructive pulmonary disease (COPD).
It aims to improve health outcomes and reduce costs by providing coordinated care
Chronic care programs offer better patient engagement, reduced costs, and improved health outcomes through increased access to care, proactive disease management, and personalized support.