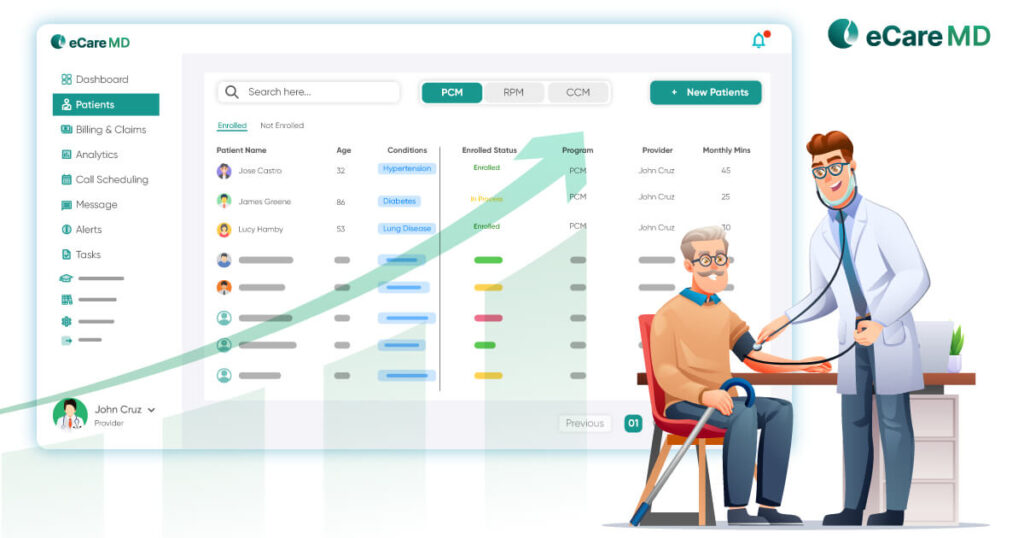
Over the years, RPM’s telehealth monitoring programs have proved to be a reliable mid-way for chronic disease management solutions. More than 21% of cardiologists have shifted to RPM for better monitoring, it has become the need of the hour of the modern-day healthcare system.
This has resulted in around a 65% reduction rate in hospital readmission for heart failure patients due to RPM.
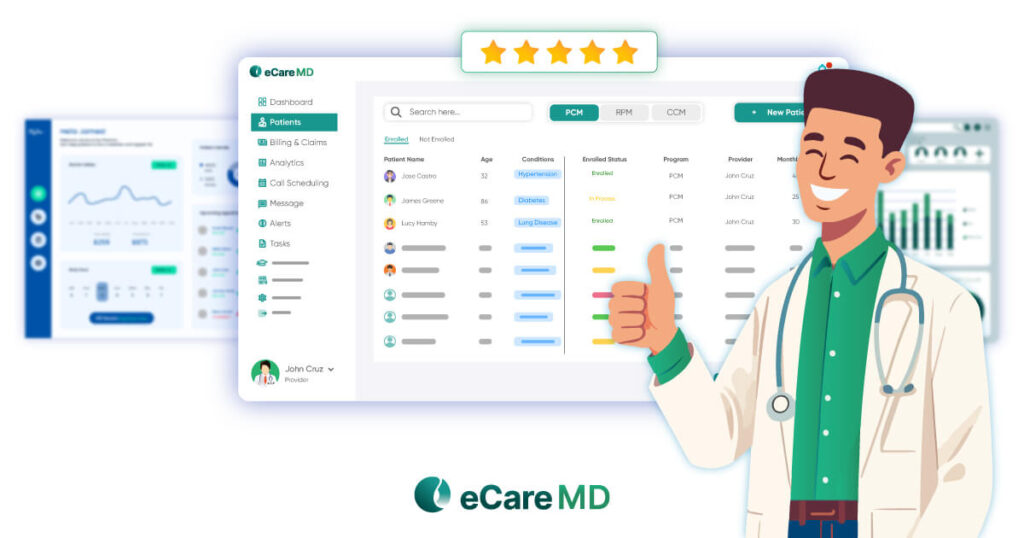
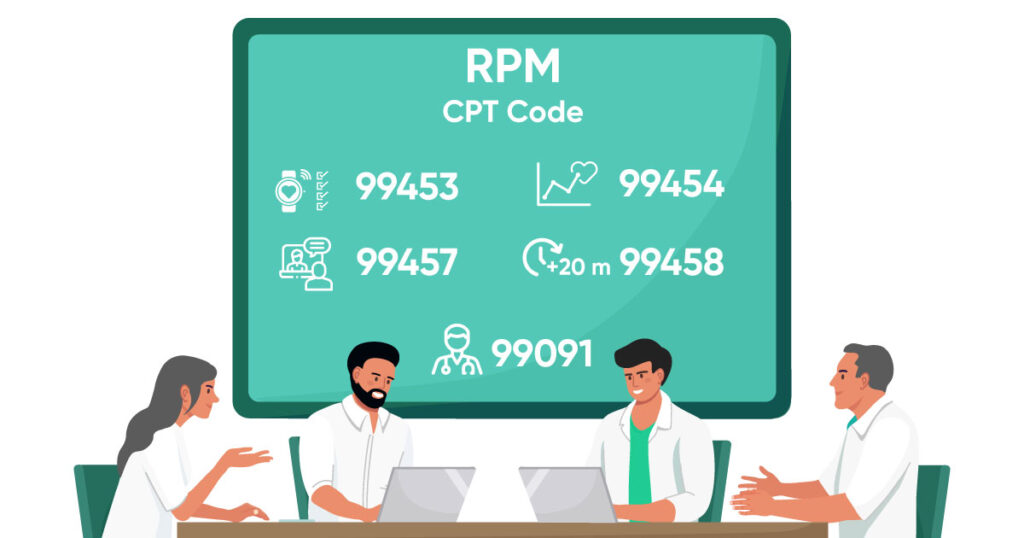
Well, let’s find out how to choose pre-customized clinic-centric remote patient monitoring software for CMS programs with specific requirements and let this blog be the free guide to choosing the right RPM technology.
Defining Program Goals and Patient Needs
How to Define Program Goals and Patient Needs for Successful Remote Patient Monitoring
Download Free GuideSelecting the Right Monitoring Technologies

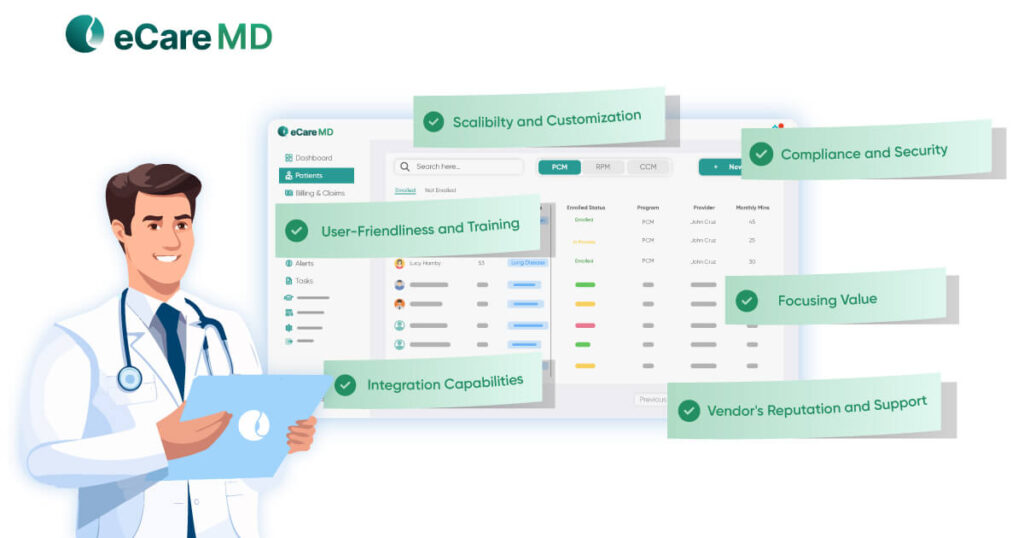
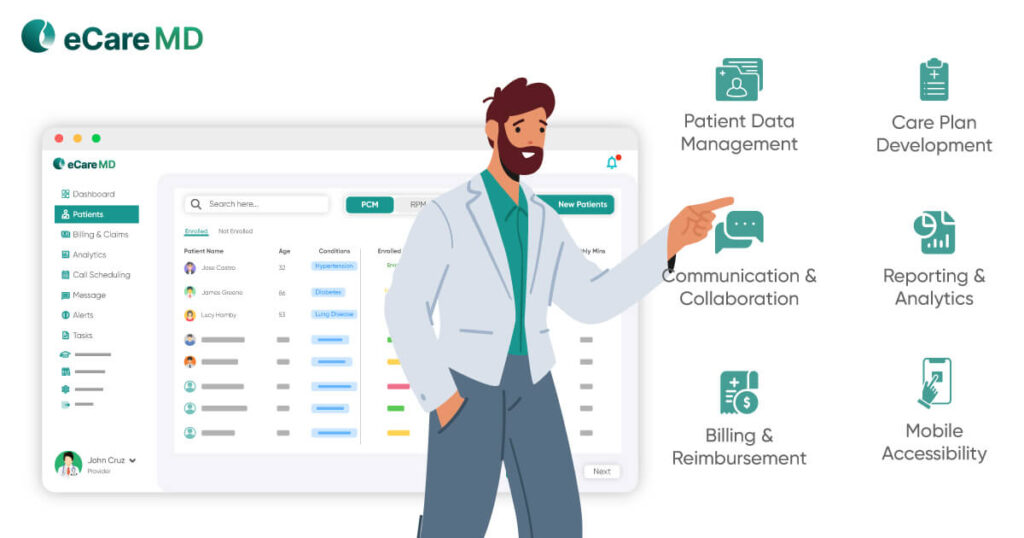
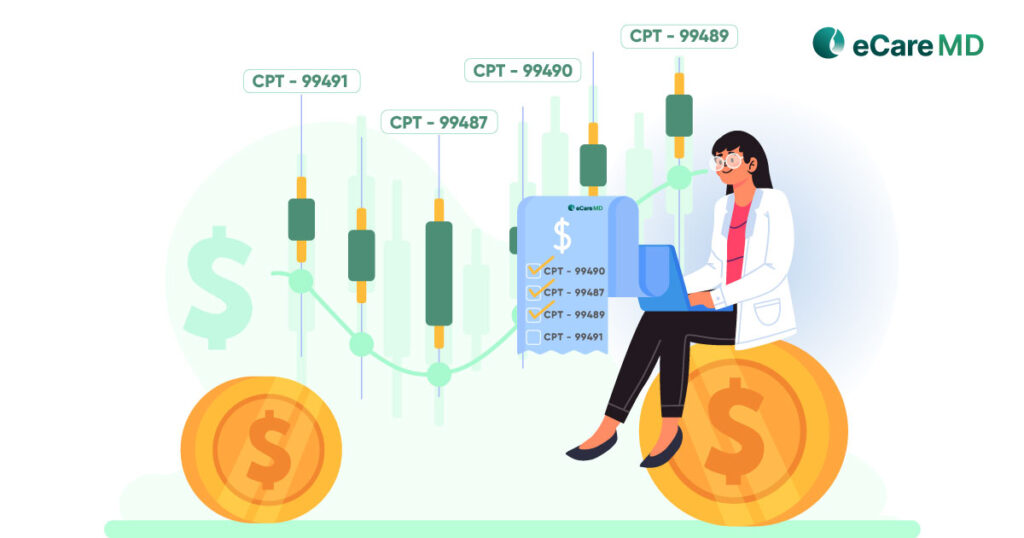
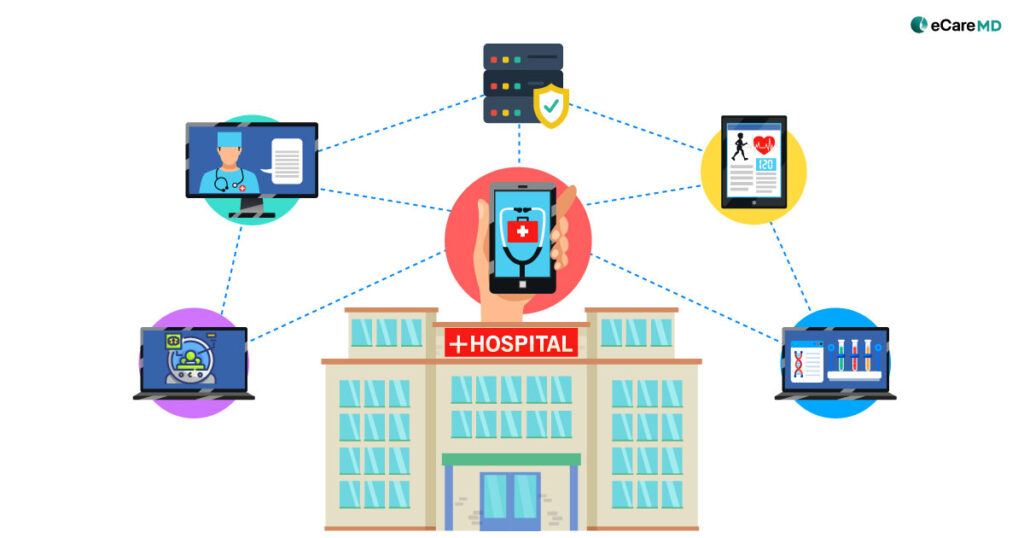
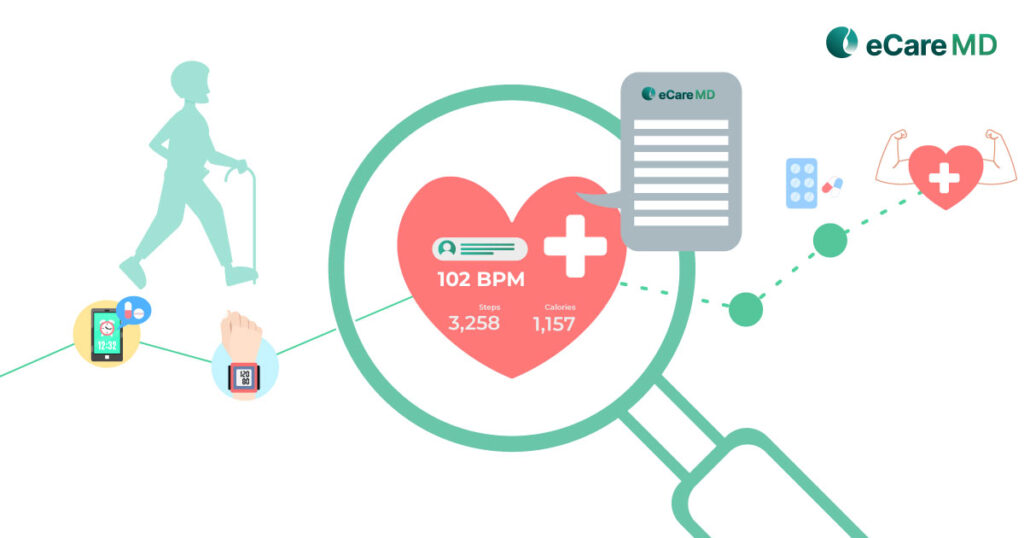
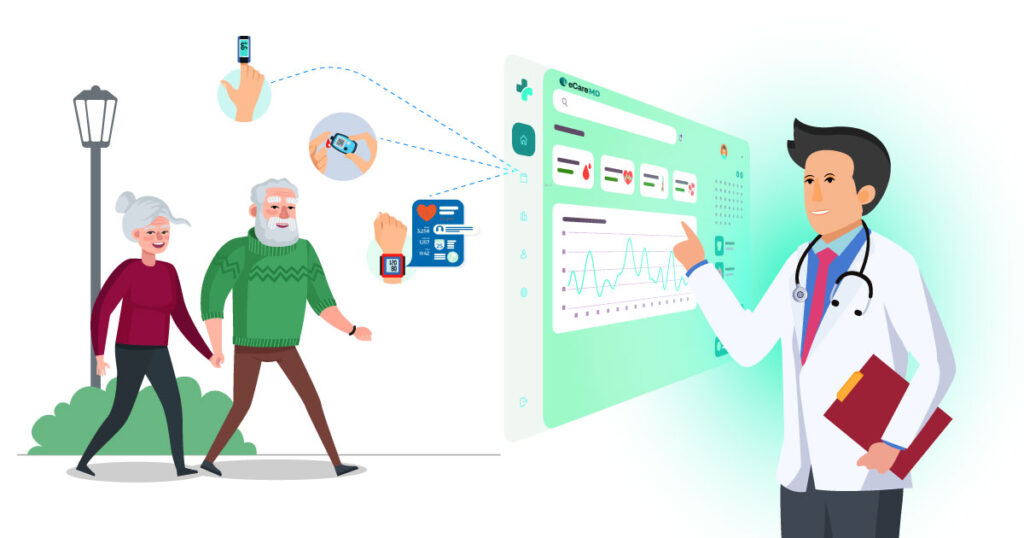
After defining the purpose of your telehealth monitoring programs and identifying their unique needs and requirements, the next step is to select the right remote patient monitoring software that uses the right technologies to drive data-backed care approaches with RPM. Here, security considerations for remote patient monitoring data is a must to maintain the integrity and transparency in your care practice.
Customizing Patient Education & Engagement Strategies

For the successful implementation of remote patient monitoring programs, it is crucial to educate patients because patient engagement is crucial for improved patient outcomes with RPM. To successfully engage patients in their care activities you need to customize your remote patient engagement strategies according to your patient population and clinical—the diseases and conditions you’re addressing—needs of your practice.
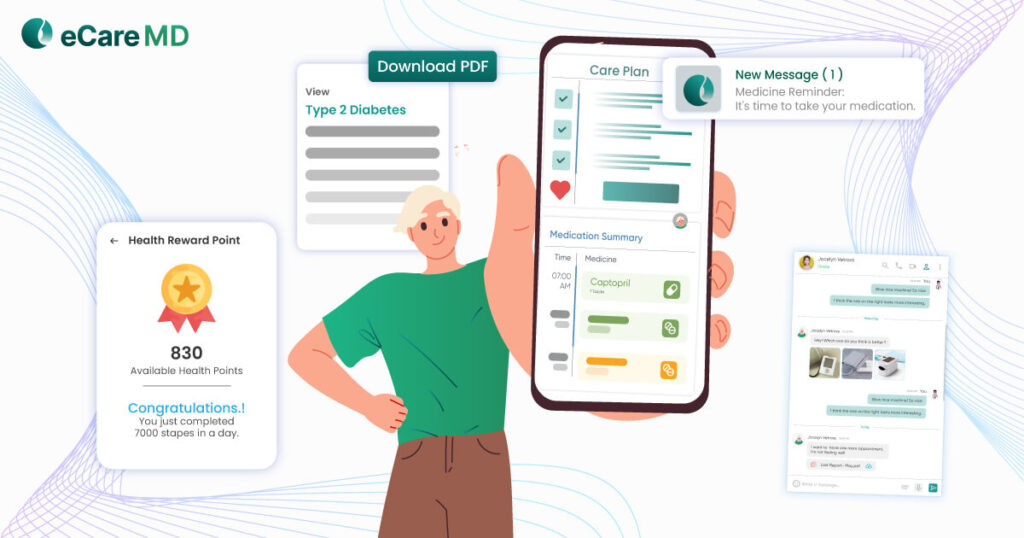
One of the effective and new ways of engaging patients in their care activities is gamification of the care elements to engage patients. Choosing the remote patient monitoring software with such features can be a good way to start gamification and further adding a reward system to keep the patients engaged can add another layer of excitement to educate and engage patients simultaneously.
Data Analysis & Program Optimization
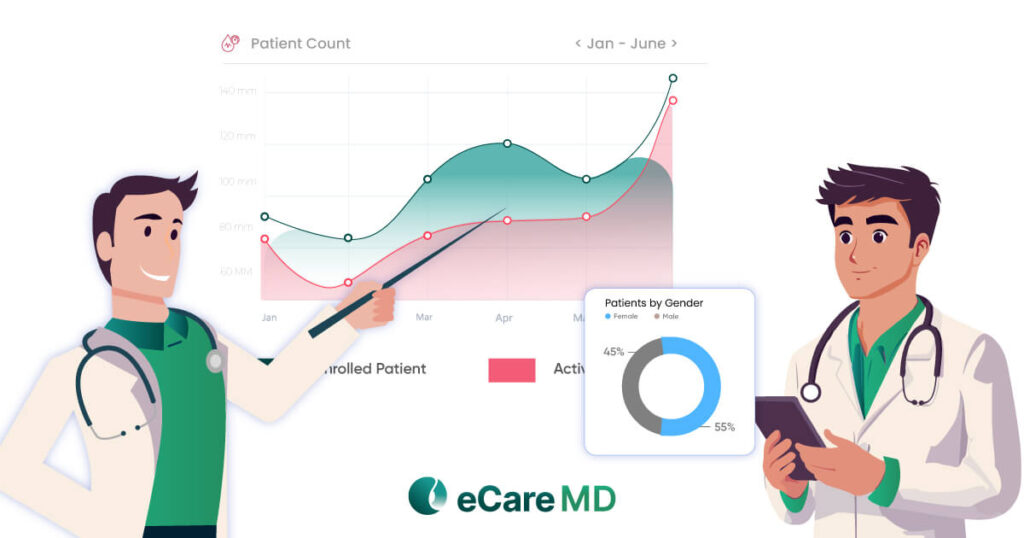
Since remote patient monitoring will enable data-driven care in your healthcare practice it can be highly beneficial for scaling and optimizing your telehealth monitoring programs. Using data analytics can come in handy to identify the areas of improvement and optimize your program for its effectiveness.
Conclusion
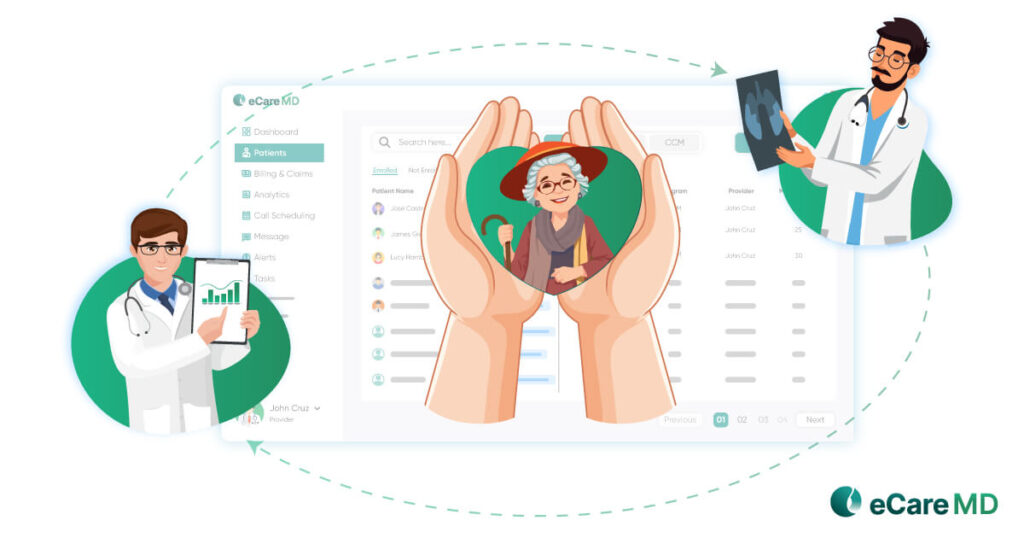
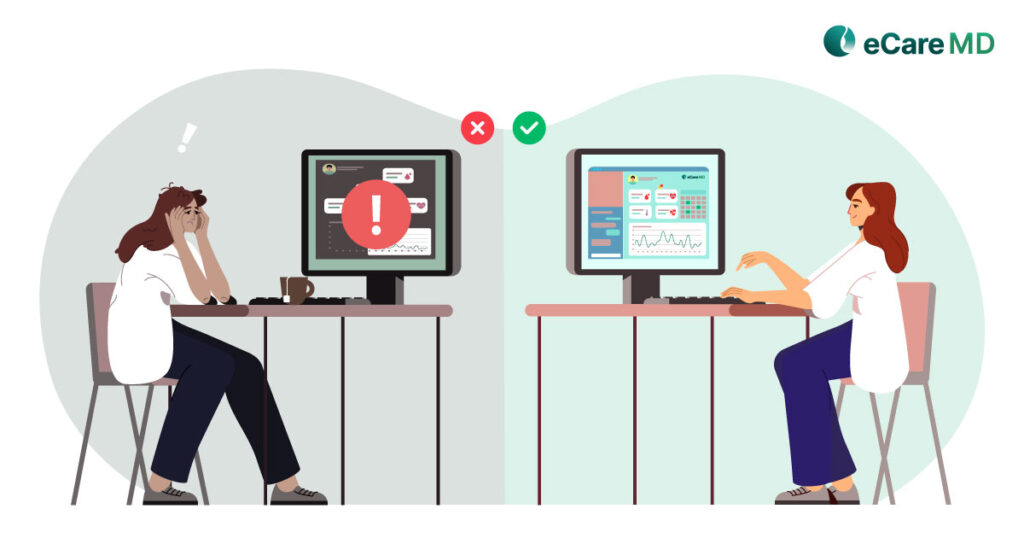
One of the major benefits of RPM for medication adherence in elderly patients has been significant in reducing the hospital readmission rate. However, to successfully implement the RPM program with CMS guidelines and while catering to the unique requirements of your practice, it is crucial for you to understand the needs and requirements of your program, clinical workflow and patient population that you’re serving.
By customizing the RPM solutions for your clinical needs will not only increase the efficiency in your practice but will directly result in improved patient outcomes with RPM. Apart from that, it will also result in improved patient engagement, increased medication and treatment adherence, reduced hospital readmission and emergency visits.
Looking at the graph and adoption rate of RPM programs in current day health care practices, it is evident that it will become an integral part of the healthcare system and play a significant role in improving healthcare delivery. So, if you’re looking for a practice-centric RPM solution to implement in your practice, click here to book a free consultation call with eCareMD’s RPM experts.
Free Consultation Call for Implementing Practice Specific RPM solutions
Frequently Asked Question’s
Here are key factors for tailoring RPM in chronic disease management:
- Patient needs: Target specific conditions (e.g., diabetes, heart failure) and tailor monitoring (blood sugar, weight, vitals).
- Technology access: Consider patient comfort with devices and internet connectivity.
- Data analysis: Set personalized thresholds for alerts and interventions based on patient history.
- Communication plan: Integrate RPM with the existing care plan and ensure clear communication between patient and provider.