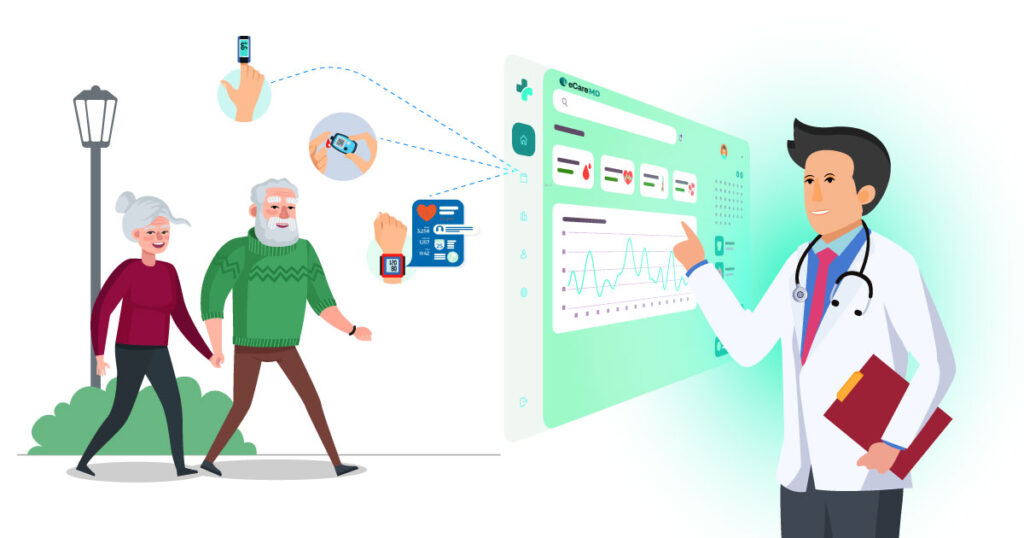
Did you know that just providing 20 minutes of Remote Patient Monitoring can generate around $1000 over 12 months?
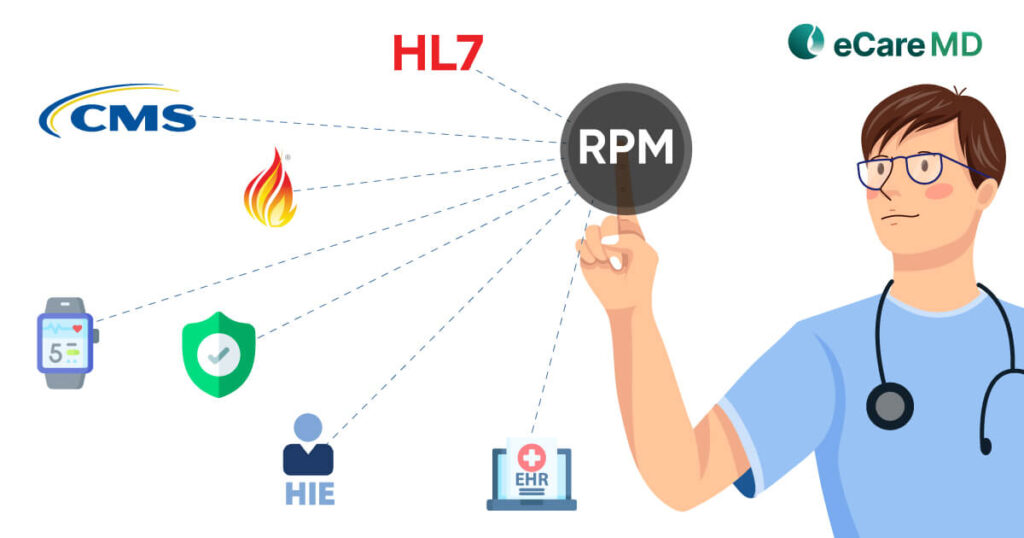
Finding the mid-way out and leveraging the power of remote patient monitoring software, CMS introduced Current Procedural Terminology codes for their programs. RPM CPT Codes have majorly streamlined the billing and coding process, but let me tell you a secret!
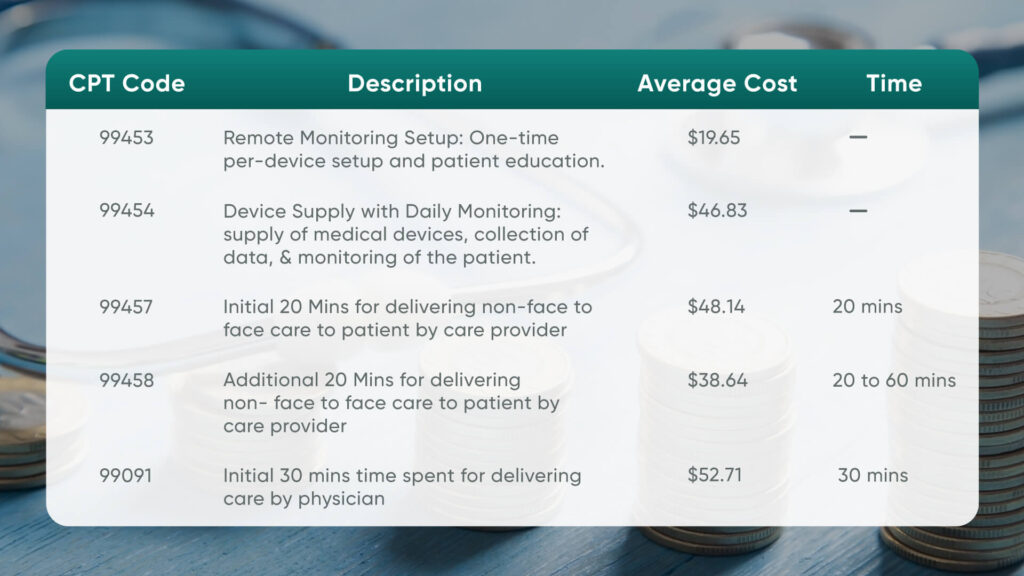
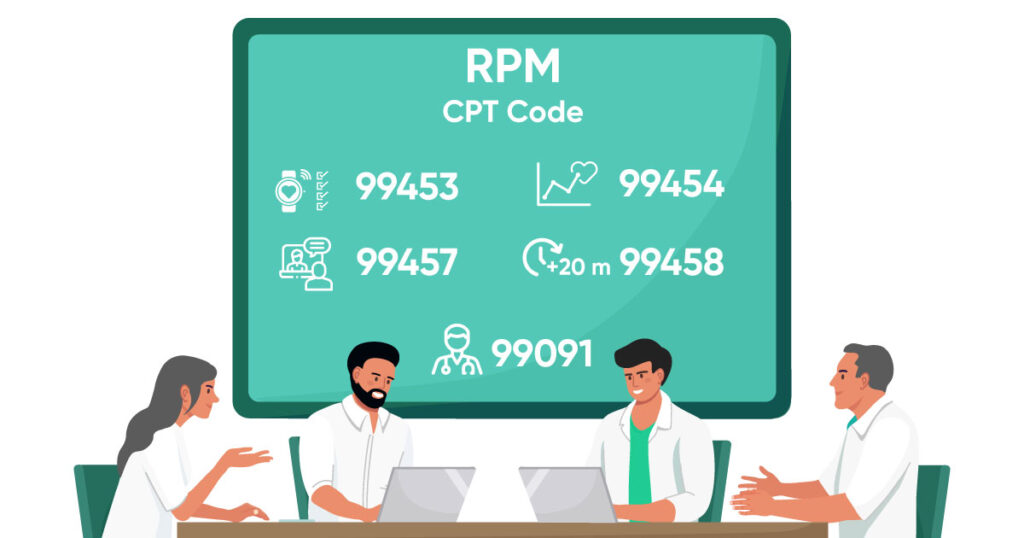
CPT Code 99453: Remote Monitoring Setup
CPT Code 99454: Device Supply with Daily Monitoring
CPT Code 99457: Remote Physiologic Monitoring Treatment Management Services
The RPM program requires care providers like physicians, healthcare providers, or clinical staff to monitor patient health for a 30-day period. This code covers the initial minutes of patient monitoring over that period of care episode.
Furthermore, this code can also be billed as an ‘incident to’ in general supervision. This means that Medicare providers can outsource RPM companies to help care managers with RPM services. This increases the effectiveness of the practice and allows providers to enroll and manage more patients in the program. However, documentation of how the time is distributed is required for complete and proper reimbursement.
CPT Code 99458: Remote Physiologic Monitoring Treatment Management Services
CPT Code 99091: Physician Care
Key Documentation Requirements for RPM CPT Codes
Remote patient monitoring billing and reimbursement consists of a lot of documentation with different elements. Some of the most common documentation elements for all RPM CPT Codes include:
- Written or verbal consent of the patient to enroll in the program.
- Documentation of the practitioner’s order for RPM services.
- The patient enrolled must document the medical necessity for RPM Services.
- Patient demographics and identification information.
- Document the type of RPM device used with all its identification.
- CPT Code 99453: For this code, you are required to document the date of delivery and training dates for patient education.Also you need to have first reading date to bill this code.
- CPT Code 99454: For this code, you are required to document 16-day data transmission and review of the data.
- CPT Code 99457: For this code, you are required to document interactive communication, time spent on each RPM service, and the content of the communication.
- CPT Code 99458: For this code, you are required to document interactive communication, time spent on each RPM service, and the content of the communication.
- CPT Code 99091: For this new code, you are required to document the time spent on RPM Service, data collection and interpretation, modifications in treatment plan, and patient-provider communication.
Coding and Billing Best Practices
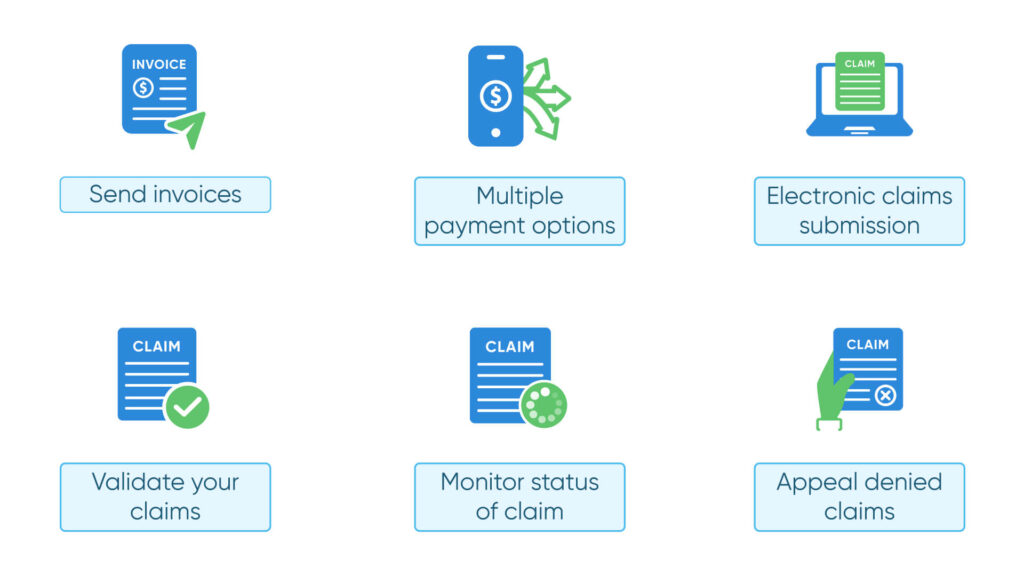
- Send invoices promptly
- Offer multiple payment options
- Use electronic claims submission.
- Validate your claims.
- Monitor the status of your claim.
- Appeal denied claims.
Conclusion
Navigating through the different requirements and documentation of RPM CPT Codes can only be done if you know the CPT Codes very well. That is why CMS requires you to effectively involve patients in their care plan and bring accuracy to coding.
The best way to navigate easily through the billing and reimbursement process is to accurately code and document every service that you provide. Doing this can help you streamline your billing process and ensure timely reimbursements. Along with that, it also reduces the chances of the claim being denied.
However, one of the things to consider when billing for CPT Codes for RPM programs is to stay informed and updated with the latest updates brought by CMS. Now, let this be your guide to RPM CPT Code moving ahead in 2024.
Frequently Asked Question’s
- Educating the patient: The staff explains how to use the monitoring device.
- Setting up the equipment: This ensures proper data collection and transmission.
- Clinician: Physician or qualified staff (supervised) can bill.
- Patient: Established patient with prior E/M service (telehealth acceptable).
- Monitoring:
- At least 16 days of device readings in a 30-day period (except suspected/confirmed COVID-19: 2 days minimum).
- Secure data management and reporting are crucial.
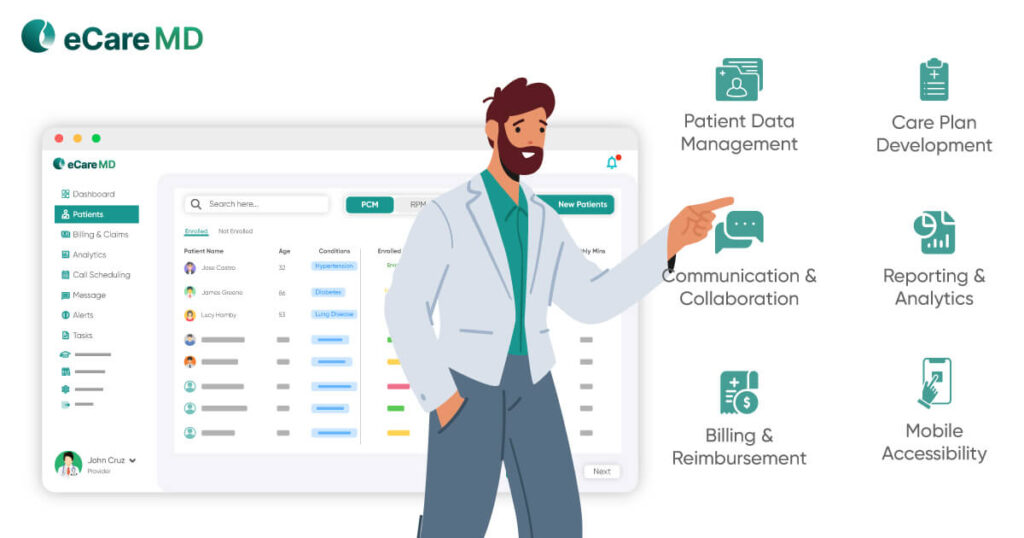
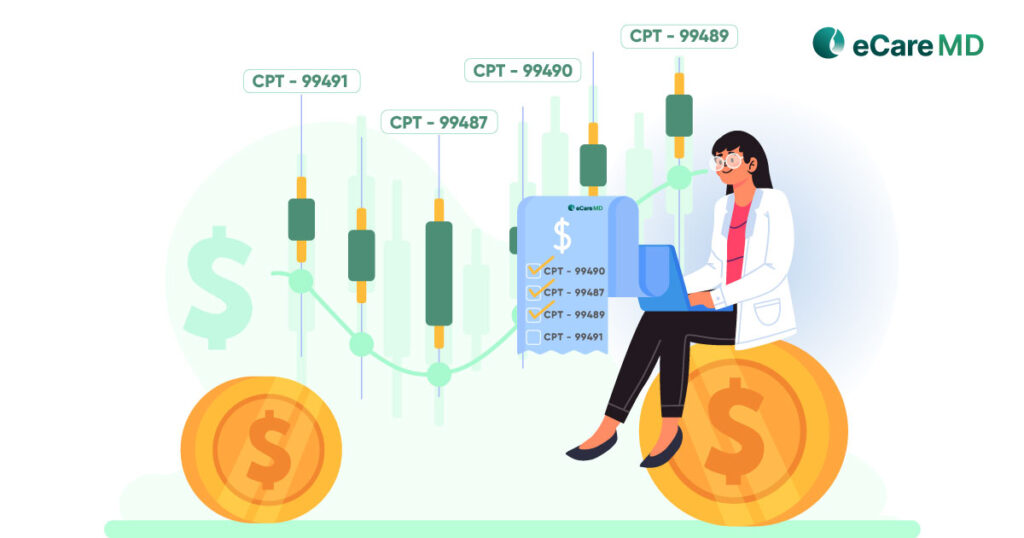
CPT codes act as a key for unlocking reimbursements for remote patient monitoring (RPM) services. Specific codes define the type of data monitored (e.g., blood pressure) and the time spent managing it. Providers use these codes to bill payers, who then reference national rates to determine the amount reimbursed for each service.
Therefore, CPT codes directly influence reimbursement by dictating which services qualify for payment and the specific value assigned to each.
- E/M services: New rules clarify reporting admission/discharge on the same day.
- Specific procedures: New codes exist for phrenic nerve stimulation, intraoperative ultrasound, and nasal nerve ablation.
- Critical care: Coding instructions for total duration were refined.
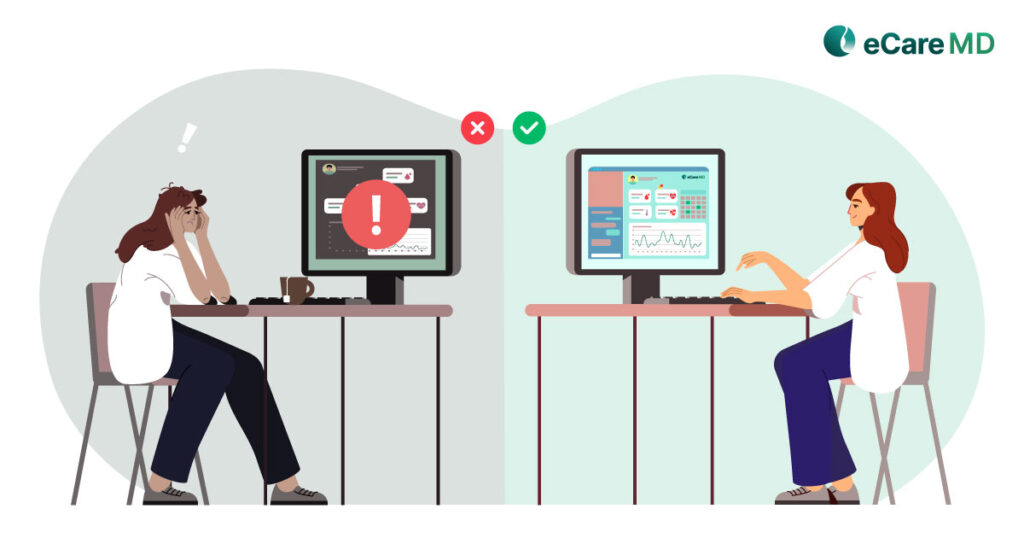
Here are some common challenges for healthcare providers billing RPM:
- Meeting Time Requirements: CPT codes 99457/8 require specific documented clinical staff time (20/40 mins) managing patient data, which can be difficult to track.
- Accurate Coding: Ensuring the chosen code (99453/4/7/8) precisely reflects the service delivered (initial setup, data monitoring, or intervention) is crucial.
- Documentation: Detailed records proving medical necessity, data analysis, and time spent are essential to avoid claim denials.
Yes, in most cases, specific CPT codes can be used together for telehealth. However, proper bundling rules apply. Combining codes like 99202-99215 (office visits) with others like 99421-99423 (online E-visits) might be possible, but only if services differ.
Remember, consulting a healthcare provider billing expert is crucial for accurate coding.