Factors Affecting Care Coordination Software Costs
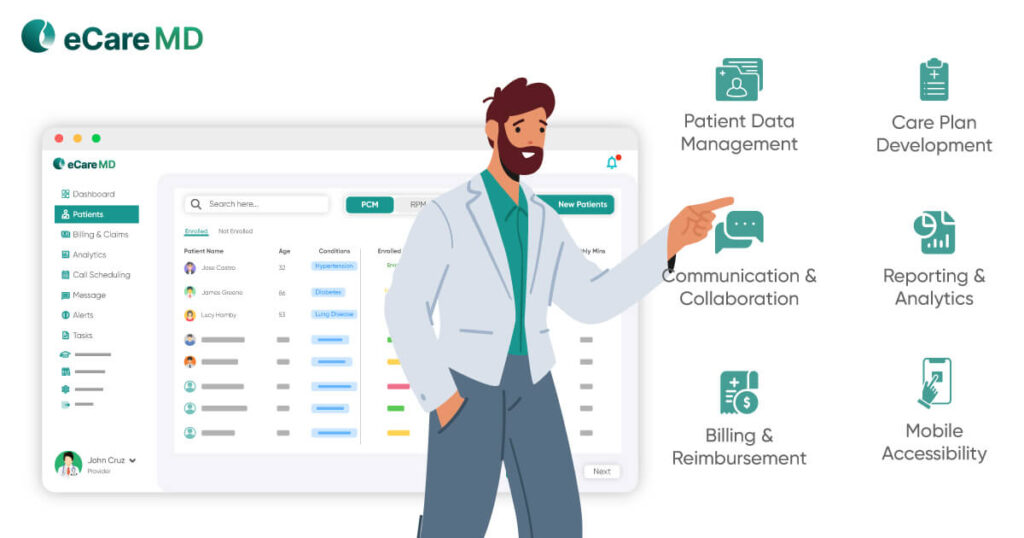
1. System Complexity & Features
2. Deployment Model
- Cloud-based RPM Software: Cloud-based solutions typically have lower upfront costs and software implementation costs. However, as you continue using the software, the recurring subscription fees can become a costly affair in the long run.
- On-premise RPM Software: Setting up the on-premise solutions has a significantly higher upfront investment for hardware, which includes servers, workstations, other equipment, and their installation. However, since it will create your own data center, it offers very low ongoing maintenance costs in the long run compared to recurring fees in cloud-based solutions.
3. Number of Patients
Download Free Guide - Care Coordination Software Cost Estimation Tool for Your RPM Program
Download NowBreakdown of Care Coordination Software Costs

1. Software Licensing
Software licensing is the core cost of the software. Since the vendor has spent significant time and money solving a specific problem for you, they are bound to charge you for their service. This is usually charged by the vendor in either an on-time fee or a recurring subscription. Depending on the vendor and the type of software you are choosing, the cost of this can change and vary significantly.
2. Implementation & Integration
The next part of the care coordination software cost breakdown is the costs associated with setting up the software for your practice. For this, the software needs to be integrated into your existing systems, and a huge amount of data is to be migrated from one system to another. These are complicated processes as they include interoperability along with the risk of data loss.
3. Training & Support
Additional Considerations
Apart from the factors affecting the care coordination software cost, here are some additional factors that might increase the costing of the remote patient monitoring software.
1. Data Security & Privacy
2. Return on Investment (ROI)
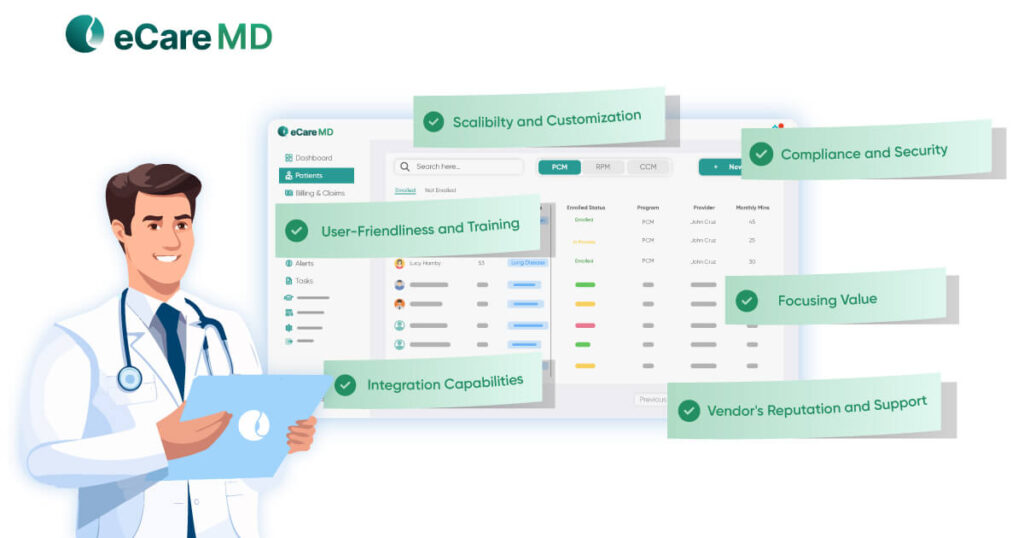
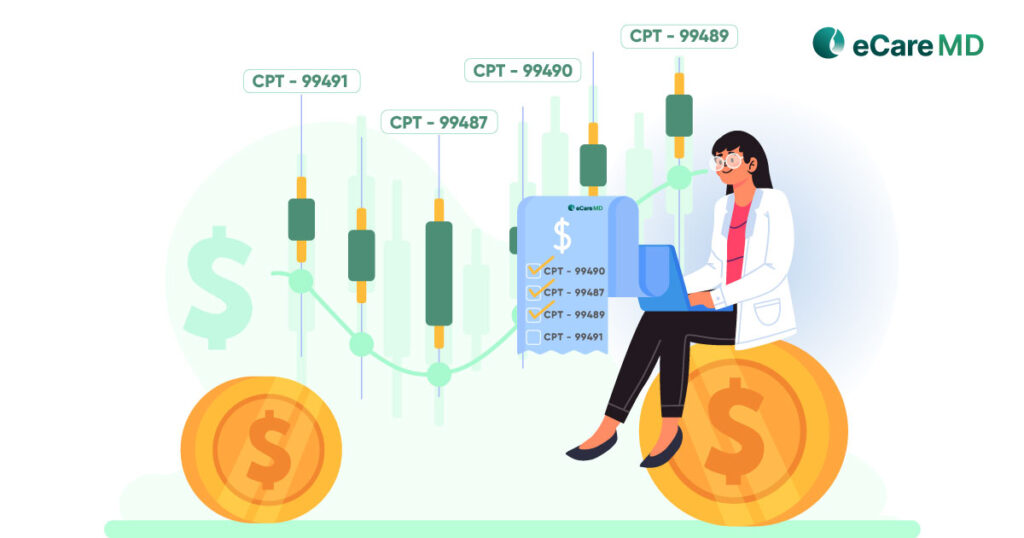
Types of Remote Patient Monitoring Software Pricing Models
- Subscription-based Models: These are typically off-the-shelf software that allows you to use the software for your RPM services. These usually work on subscription models where you have to pay a subscription fee monthly or annually.
- Per-user Licensing: To make the software affordable for everyone, vendors also have a per-user licensing model, where you pay the vendor for the software as per user.
- Usage-based Pricing: Also known as the per-feature subscription pricing model, where you would have to pay the vendor for every feature you use within the RPM software.
- Customized Pricing Structure: Most healthcare providers look for customized solutions; this is where the development, maintenance, and support costs are added.
Conclusion
RPM has created a win-win situation in the healthcare industry, moving from a traditional to a digital landscape. While software is the core part of it, deciding the cost of the RPM software can be even more daunting for someone like you. Moreover, having a strategy while making decisions in selecting the right RPM software for your practice can define the future roadmap for your CMS RPM program.
While the RPM tides are picking up pace in modern-day healthcare, let this blog be your guide in choosing the right RPM software for the right price.
Free RPM Software Cost Comparison Checklist
Frequently Asked Question’s
Care coordination software costing has four different types of pricing models:
- Subscription-based pricing model
- Per-user licensing
- Usage-based Pricing
- Customized Pricing Structure
Three factors to estimate your RPM care coordination software cost:
- Features: Basic options start around $ 1 per month per patient, while feature-rich options can reach $ 8 per month per patient.
- Patients: Per patient, pricing might be better for smaller practices, while flat fees can be cost-effective for larger ones.
- Services: Full-service management by a third party can cost $20-$30 per month per patient.
Considering these hidden costs of care coordination software include:
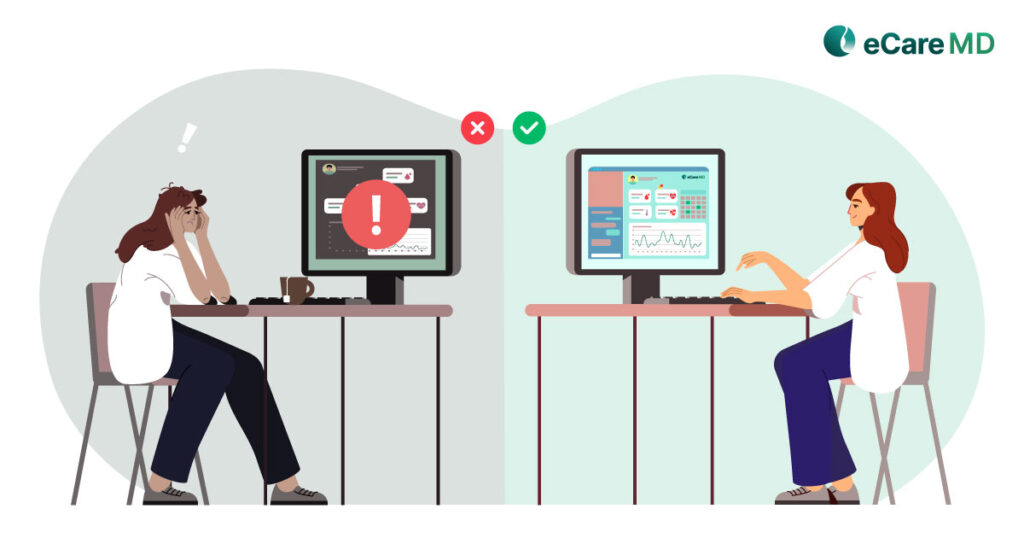
- Confusing software can slow down your staff and cost you money.
- Fees per patient can add up quickly for bigger practices.
- Training and extra help can be expensive.
- Choose software that’s easy to use and has clear pricing to avoid hidden costs.
Here are some resources to help you choose care coordination software:
- Industry review sites: These offer expert comparisons and user feedback on various software options.
- Vendor websites: Explore features, pricing, and case studies to understand how each software fits your needs.
- Professional associations: Seek recommendations and best practice guides from healthcare organizations.
- Software demos: Get firsthand experience by trying out different software options.