However, healthcare professionals, being so used to the traditional fee-for-service model, found the transition to a value-based reimbursement model more difficult. Moving ahead as value-based care gained momentum, implementation of it with Remote Patient Monitoring made sense but proved to be challenging for providers. But indeed, the benefits of RPM for value-based care have been exceptional, making them a match made in heaven.
But is implementing RPM for value-based care challenging? What are the challenges of using RPM and value-based care?
Join Free Webinar - Maximizing Reimbursement with RPM: Best Practices for Value-Based Care
Join nowWhat is Value-Based Payment in Healthcare?

What is Value-Based Care with RPM?
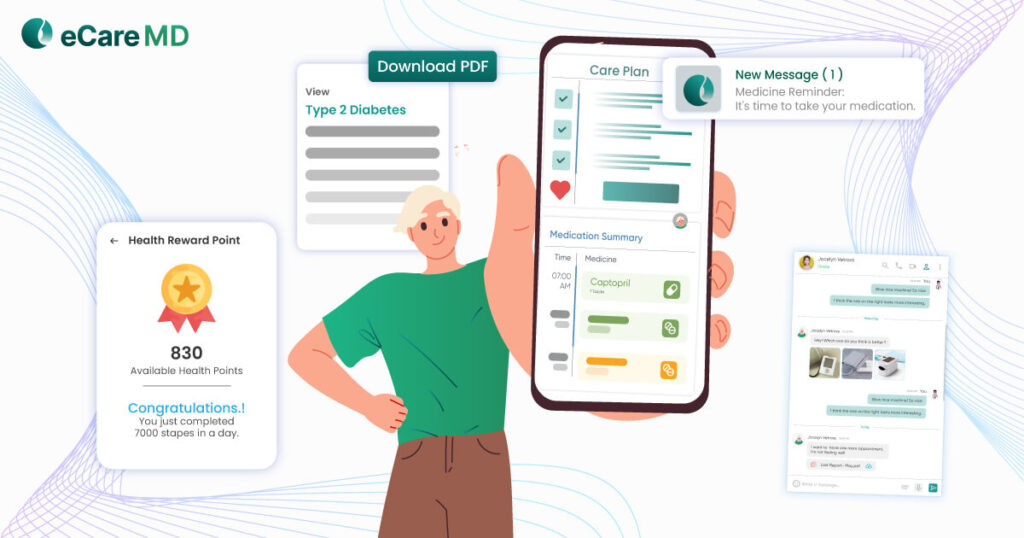
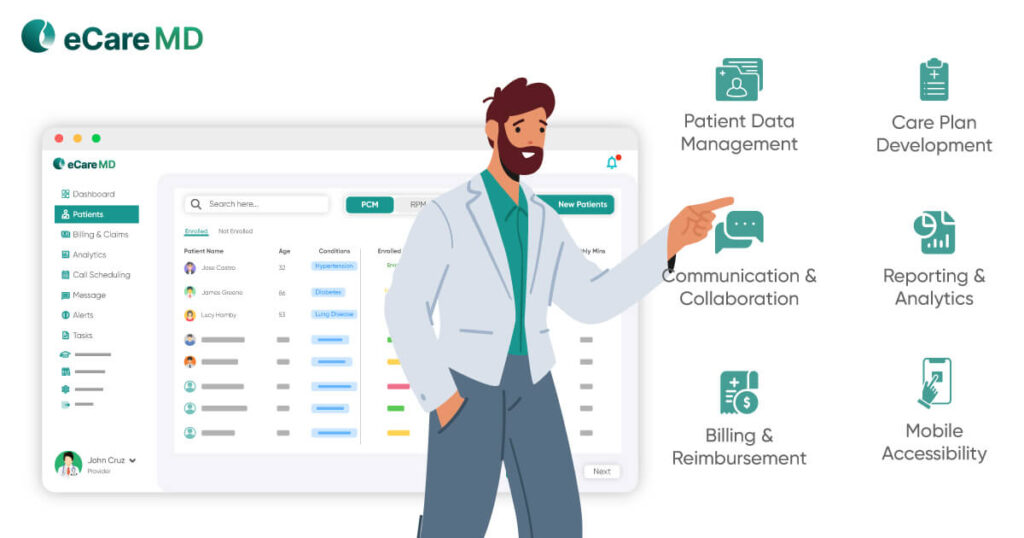
In a nutshell, remote patient monitoring is a way of monitoring a patient’s condition and the outcome of a typical healthcare practice. With this, gathering crucial patient vitals in real-time, like blood pressure, heart rate, glucose levels, etc., becomes much easier.
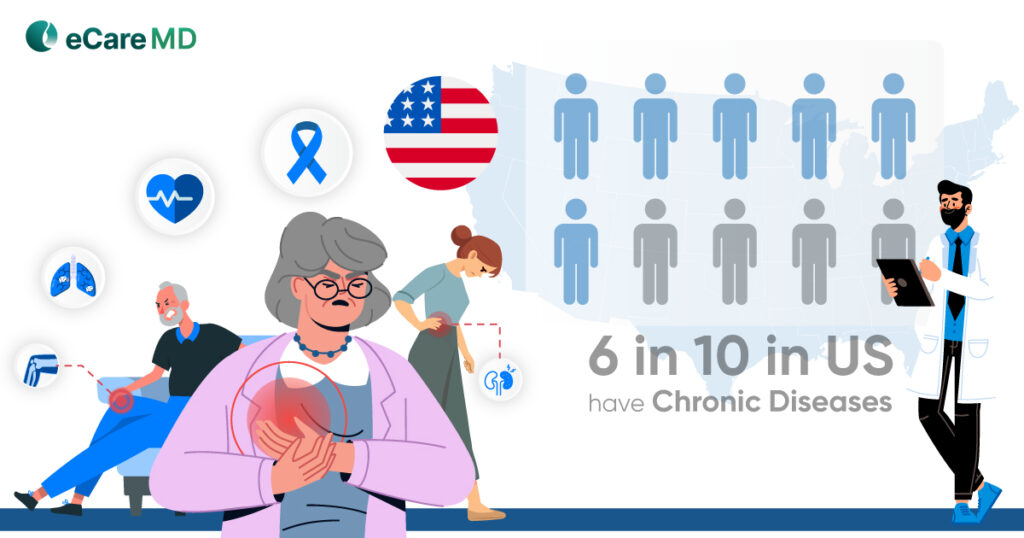
Improving Chronic Disease Management
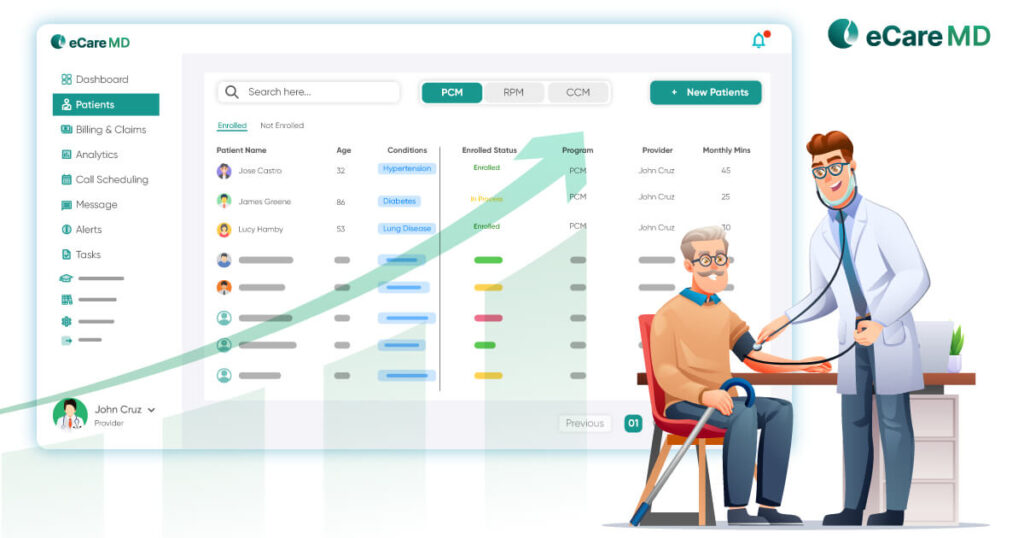
The major USP of remote patient monitoring is that it directly instills data-based decision-making into your healthcare practice. This enhances chronic disease management, where value-based care contributes to increasing clinical efficiency with RPM.
Enhancing Patient Engagement & Self-Management

Increasing Clinical Efficiency
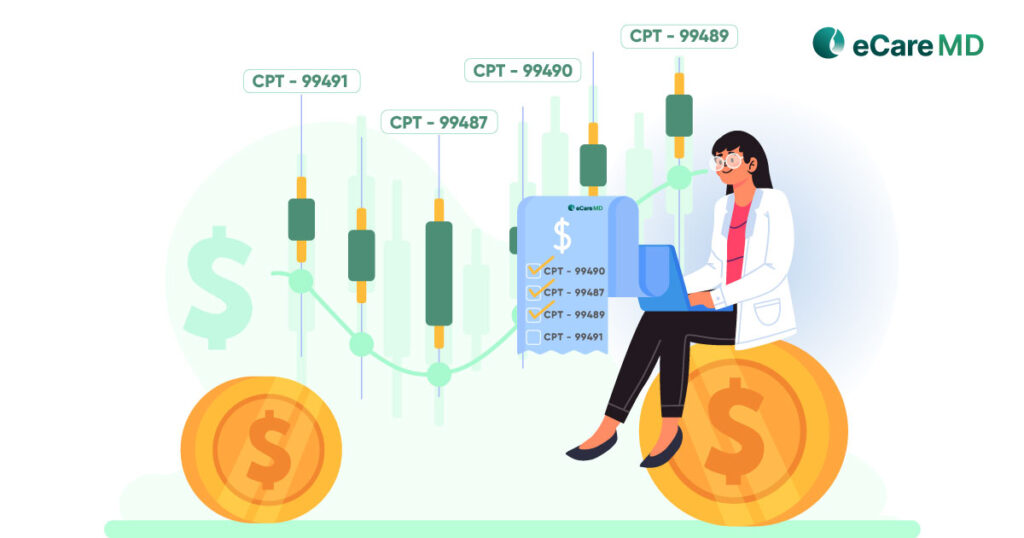
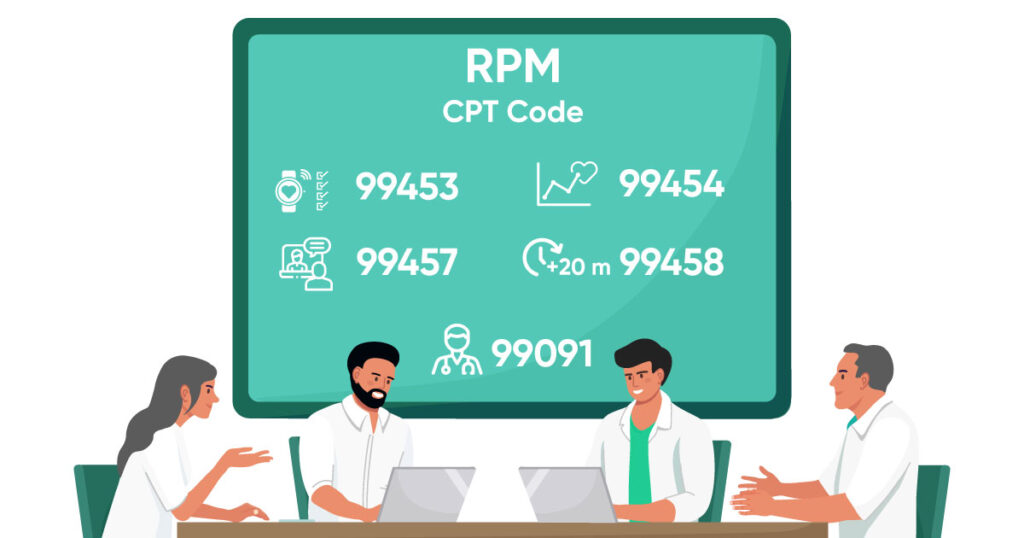
Demonstrating Value in Reimbursement
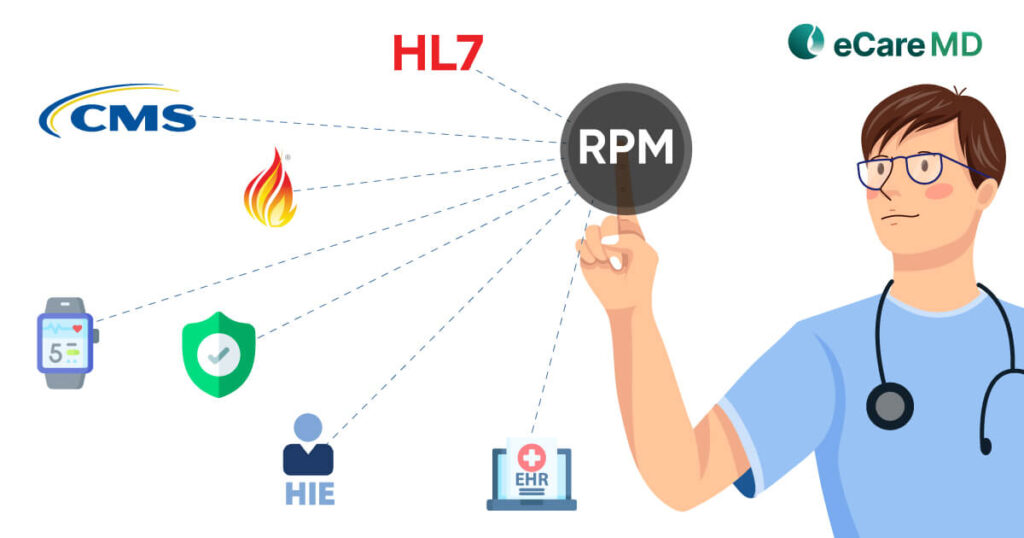
As mentioned earlier, RPM and value-based care are a match made in heaven, it is because of their alignment of the factors or quality metrics. Meaning that the quality metrics used in value-based reimbursement are the same as those used for measuring the success rate of remote patient monitoring programs.
Tips & Tricks to Maximize Reimbursement in RPM
Conclusion
Value-based care is gaining momentum as evidence-based practices are considerably growing in the modern-day healthcare system. Furthermore, with RPM, providing value-based care can be streamlined and effectively brought into practice. To implement that into your practice, have a strategic plan to start your RPM program and use that data to improve patient health outcomes.
Value-based care practices can not only help patients reduce the cost of care but also keep them at the center of the curation of care plans. This helps engage them effectively with their care plan and positively impacts patient outcomes. Furthermore, value-based care practices are the future of healthcare as they aim to improve the quality of care and efficiency of healthcare facilities effectively.
Last but not least, if you’re looking for a way to instill value-based care with RPM, then click here to book a free consultation call.
Download Free Checklist - Checklist to Implement RPM for Value-Based Care
Download nowFrequently Asked Question’s
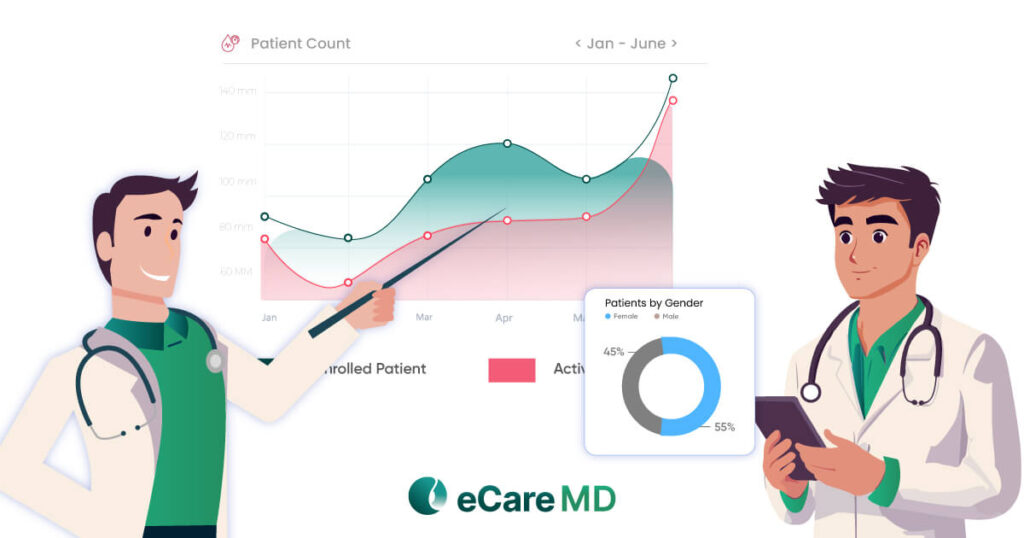
Studies show RPM reduces hospital readmissions by 20% for heart failure patients, lowers healthcare costs by $5,000 annually for diabetics, and improves medication adherence for COPD patients. These factors contribute to better patient outcomes and cost reduction in value-based care models focused on preventive and efficient care.