Chronic diseases like heart disease, stroke, and Alzheimer’s disease are the leading cause of death in the United States. Most of these deaths could have been easily avoided with appropriate preventive care or implementing a chronic care management program.
The chronic care management program was introduced in 2015 by the Center for Medicare and Medicaid Services (CMS) to reduce the piling burden of chronic conditions on healthcare providers. However, many care providers hesitate to start a CCM program for fear of failure.
Furthermore, those who implement such programs into their practice usually end up making mistakes that lead to the failure of the program. Though the implementation of the program can be tricky, it can be easily navigated with proper strategy and planning.
To help healthcare providers in the successful implementation of the CCM program, here are the common pitfalls in CCM that one must overcome. This blog will cover the most common mistakes and how to avoid them.
Common Pitfalls in CCM Program Management
The most common mistake that healthcare providers make is that they first purchase the chronic care management software and then try to implement it into the system. This makes it difficult for the staff and providers to adapt to the system and workflow usually gets disrupted.
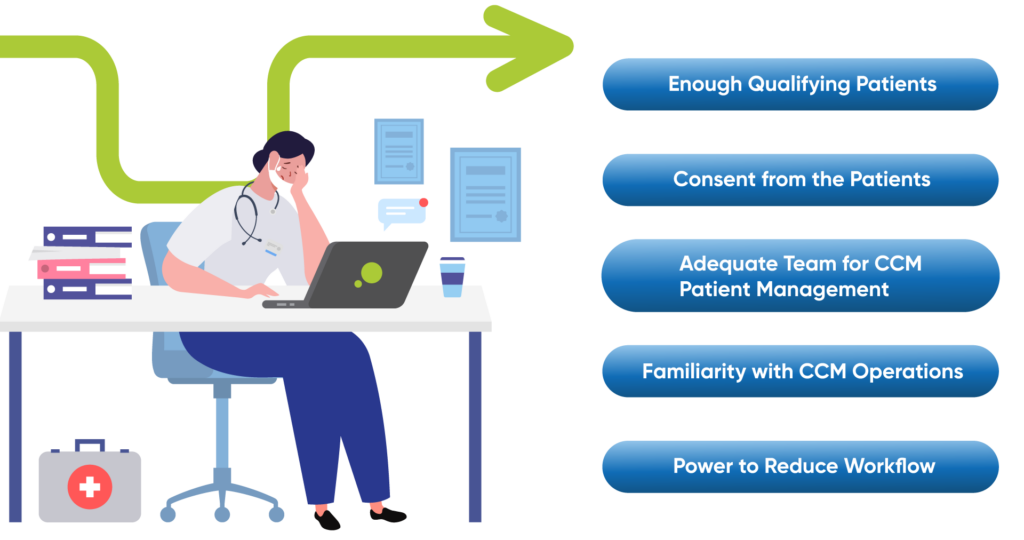
So, to avoid the most common mistakes in CCM that follow, asking these five questions can easily help you avoid the common pitfalls and challenges in CCM and successfully implement the chronic care management program.
1. Do you have enough Qualifying Patients?
CMS has set clear guidelines for the patients qualifying for the chronic care management program. Often, people starting the program make the common mistakes in CCM to start without identifying the patient population. Two major components of these guidelines are:
- The patient must be having two or more chronic conditions to be eligible for the CCM program.
- The patient’s chronic illness must be prolonged for at least a year or last a lifetime.
Though this seems a very obvious consideration, it can easily escape the eyes. Having enough qualifying patients under the program, in the beginning, is crucial for the sustainability and success of chronic disease management in the long run.
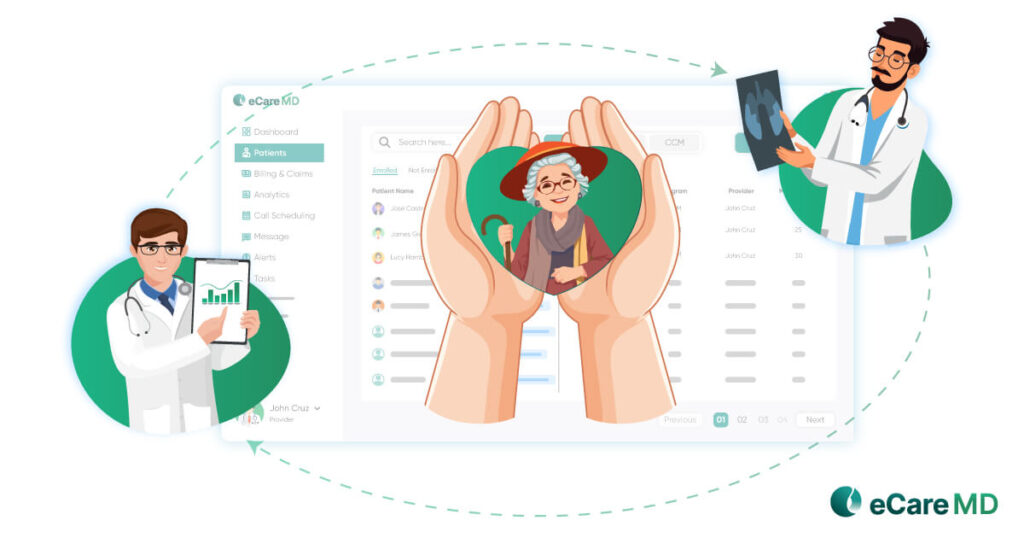
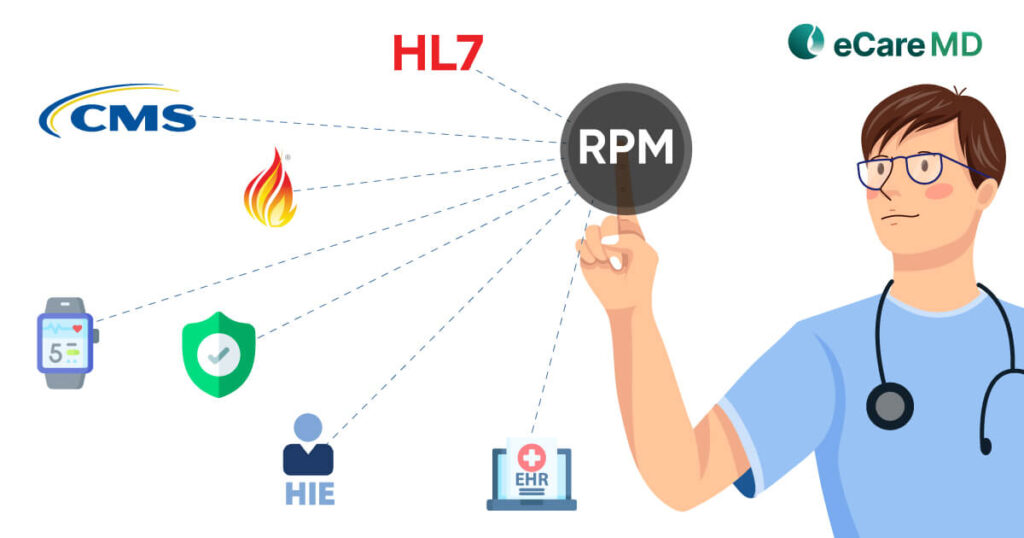
Furthermore, finding enough qualifying patients for chronic care management is not difficult, as one in four American adults has more than two chronic conditions, as per CMS. However, it is a time-consuming task, and leveraging the power of EHR/EMR can help you easily identify patients who can qualify for the CCM program.
2. Do you have Consent from All the Patients?
Once you have identified the patients who qualify for your chronic care management program, it is time to enroll the patients under the CCM program with their consent. As per the guidelines set by CMS, verbal or written consent from the patient stating they are enrolling in the program is enough to enroll them.
The mistake that many healthcare providers commit here is that they presume that all the eligible patients are enrolled under the CCM program. This can not only be the first step towards failure but also can bring the healthcare providers in legal trouble.
Furthermore, getting the patients to enroll in the CCM program is challenging. Personal consultations and phone calls are some of the most effective CCM best practices to onboard patients. However, the time consumed in this process further elongates the implementation of the program. Other ways to make patients aware of the program can be by sending automated personalized text messages and emails.
A proactive strategy to get patients on board with the program is to explain to them the benefits of the program and how it can help provide better care while reducing the overall spending on chronic care.
3. Do you have Sufficient Staff to Manage CCM Patients?
Chronic disease management is an elongated program of a healthcare practice specifically dedicated to the care of chronically ill patients. Managing the patients under the CCM program can be challenging and even overburdening the healthcare staff.
According to CMS, a care manager or care coordinator is required or a chronic care management program. Furthermore, the care manager should be a certified practitioner. Here are some of the practitioners who can be a care manager:
- Registered Nurse
- Licensed Practical Nurse
- Certified Medical Assistant
- Health Coaches
Usually, the clinical staff are designated as care managers and are asked to manage a huge number of patients monthly. Considering even a minimum of 20 minutes per patient can increase the burden on the staff. This can not only affect the efficiency of the practice but also impact the health outcomes of the patient.
Being prepared with well-educated and dedicated staff for the CCM program can contribute significantly to its success. Also, it’s always better to have sufficient staff to improve the efficiency and success of chronic disease management in your practice.
4. Do you have an Understanding of How to Run a CCM Program?
Getting chronic care management software and incorporating the CCM program into the practice is easy. However, the trouble starts when it comes to running the program successfully. Understanding the intricacies of the program is important as many providers and staff members find the digital transition difficult to adapt to.
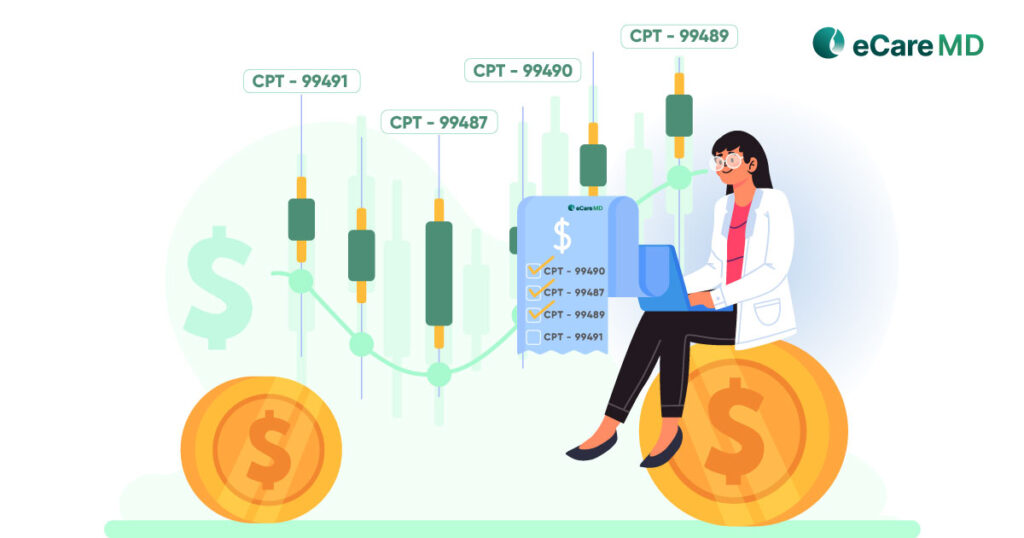
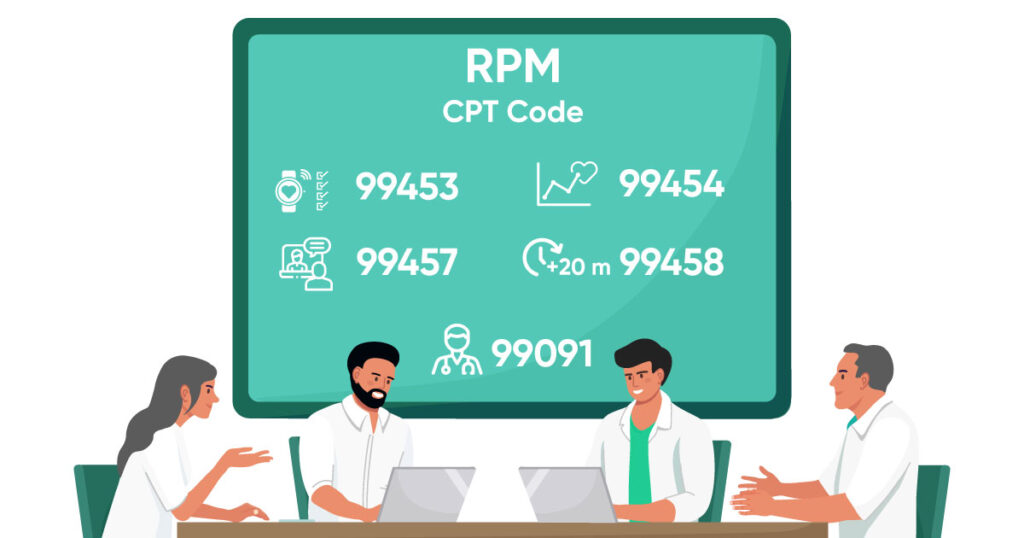
To run a successful CCM program, it is important to understand the guidelines set by the Center for Medicare and Medicaid Services. Though providing care to patients is easy, abiding by the care provisions and billing is where the success of the CCM program depends on.
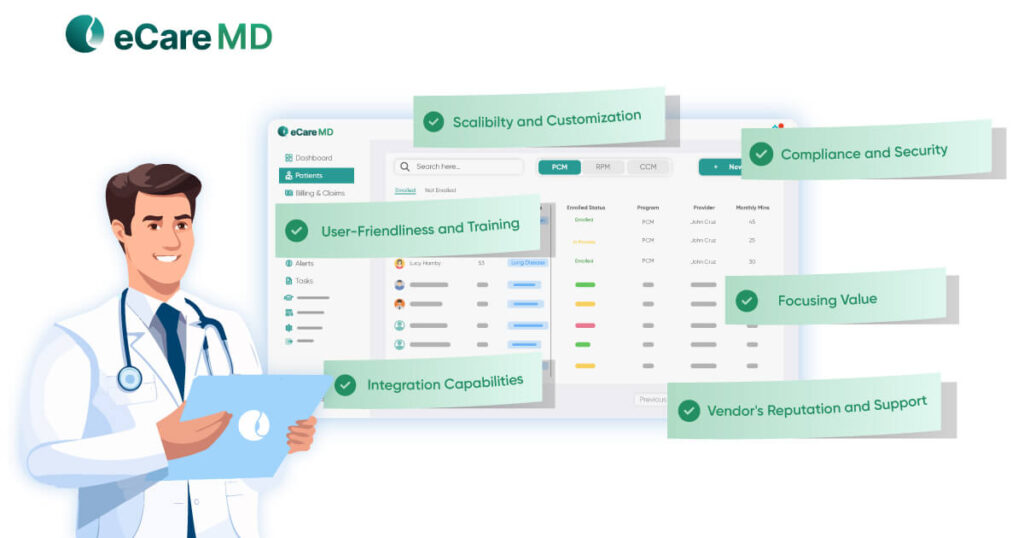
5. Is the CCM Software powerful enough to Reduce the Workload?
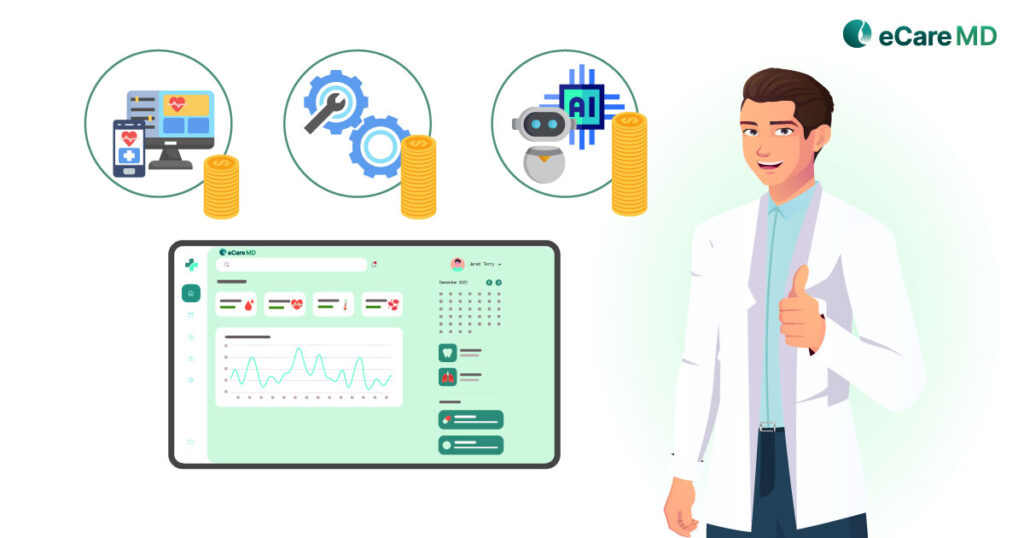
Now, let’s suppose you have ticked all the check boxes mentioned above and are ready to start the chronic care management program. However, no matter the quality of care you provide, if the chronic care management software is incompatible with meeting your needs and demands, the program is bound to fail sooner or later.
You need the CCM software to meet the unique requirements of the chronic care management program. Furthermore, the software should reduce the healthcare provider’s workload and not make the entire process complicated.
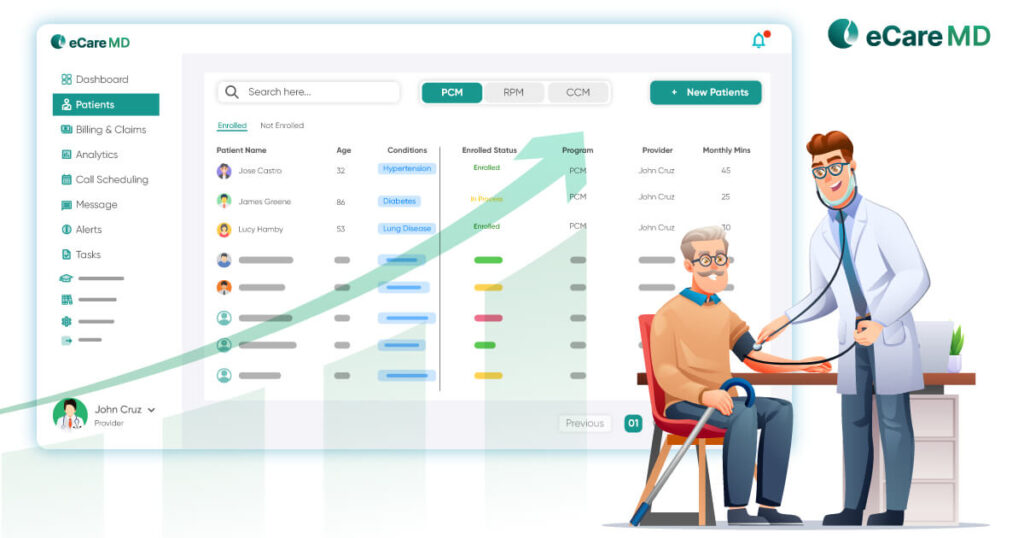
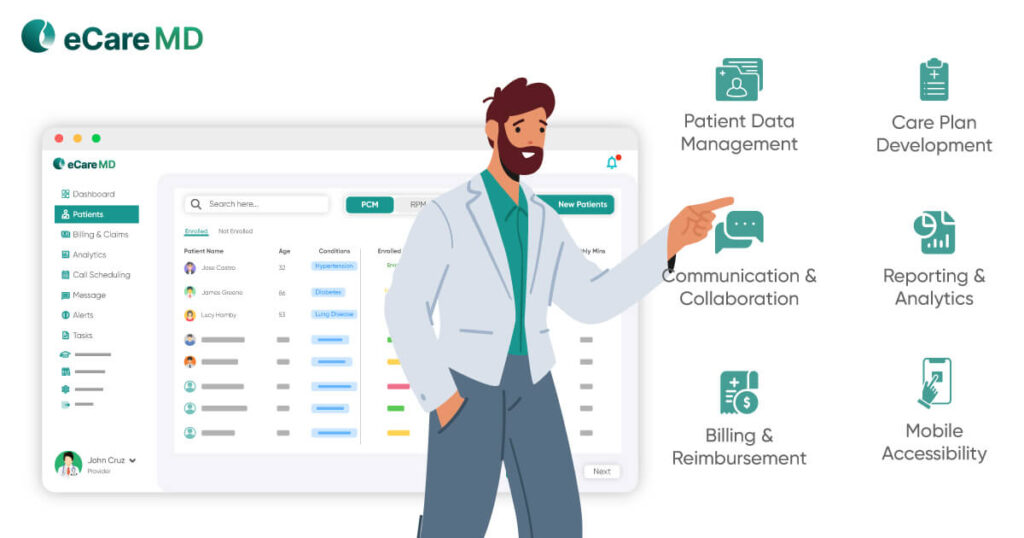
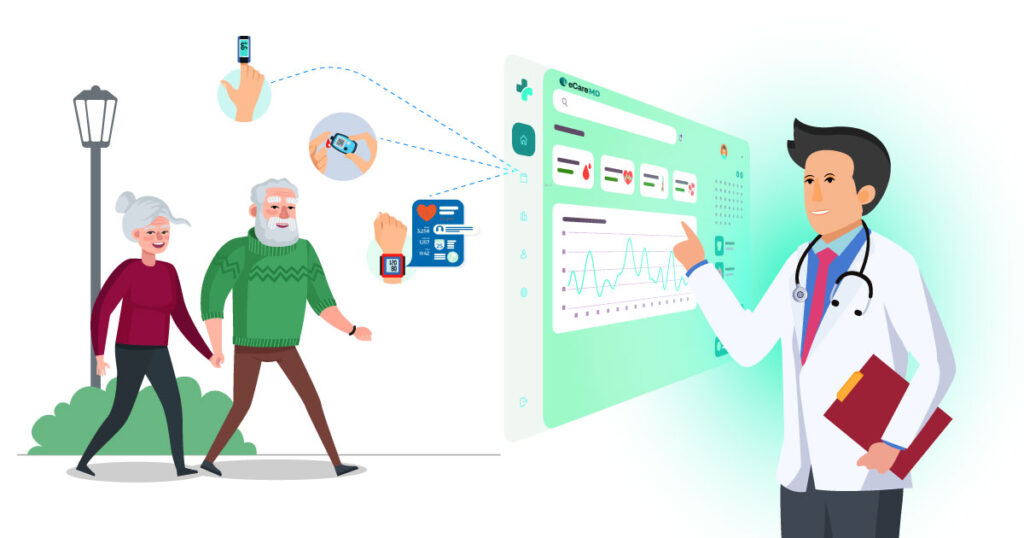
A good chronic care management software can assist in:
- Patient appointment scheduling.
- Automated time logging and tracking.
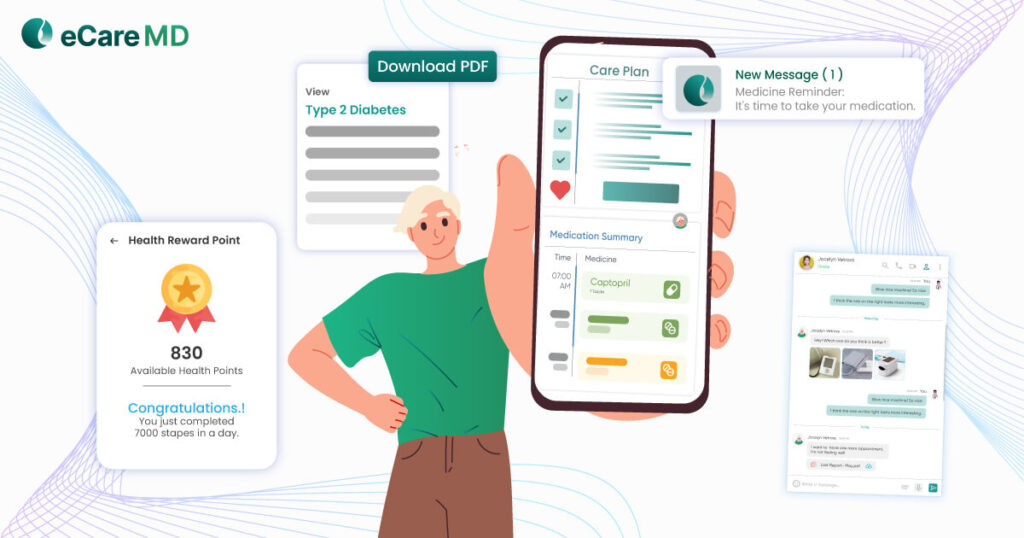
- Creation and management of patient-centric care plans.
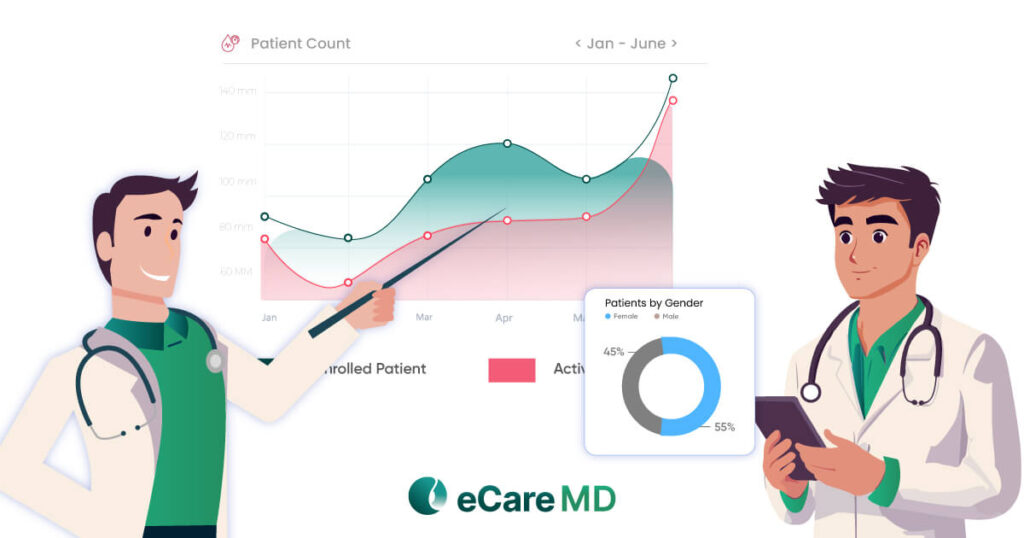
- Data analytics and reporting for the program summaries.
- Better management of CCM programs with detailed dashboards and worklists.
- Data collection and analysis to notify alerts.
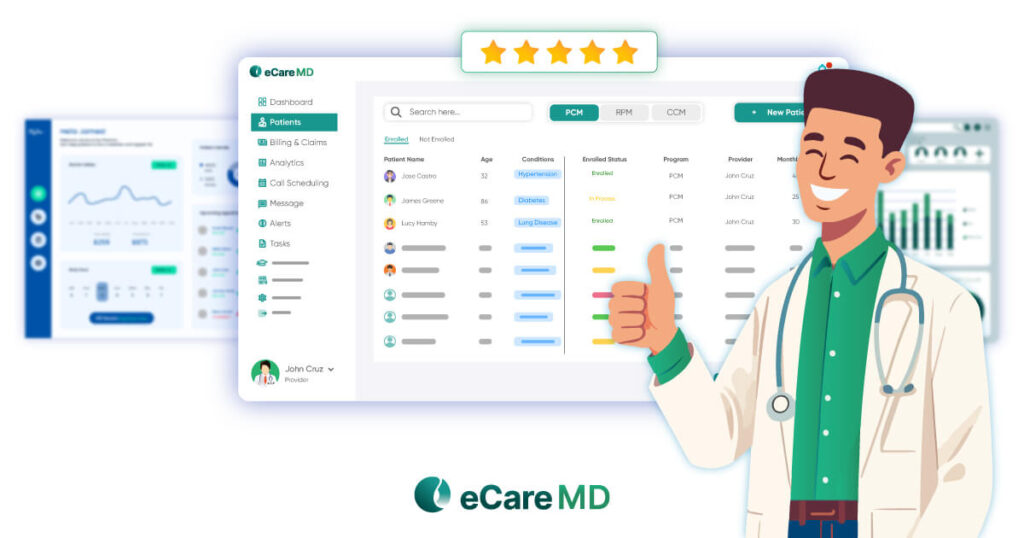
Reviewing the chronic care management software in the market to meet your needs can help you find the right CCM software, like eCareMD, for your practice.
Communication Challenges
The success of any program depends on communication, especially in chronic care management programs. Since it lacks physical one-on-one conversations between physician and patient, establishing clear communication channels and workflow is where most healthcare practices starting the CCM program struggle.
Poor communication leads to gaps in care delivery and the chances of missed appointments. Along with that, it also increases the margin of error in diagnosis and ultimately leads to poor patient engagement, patient satisfaction rate, and health outcomes.
To avoid pitfalls in communication, your CCM software should have secure and real-time communication channels. Instantly notifying the care team members and the patient is an effective way to overcome communication challenges.
Download Free CCM Feature Checklist for Effective Communication Checklist
Download nowPatient Engagement Pitfalls
Another pitfall in chronic care management is engaging the patient with their care journey. Lack of patient engagement over virtual care has seen many patients quitting the program mid-way through the journey. Keeping the patient engaged in their care journey is necessary for achieving the care goals since it contributes to informed decision-making, better treatment adherence, and active involvement in the care journey.
The lack of interest in providing care to the patient can demotivate the patient and lead to breaks in communication. Implementing robust patient engagement strategies in the program with the help of CCM software increases patient engagement. One of the effective ways for providers to achieve higher patient engagement is by giving a human touch while communicating with the patient. For instance, starting the conversation by talking about the patient’s day-to-day activities can not only make the patient feel more valued but also add a human touch to the process of care delivery.
Data Inaccuracies and Documentation Pitfalls
Despite all the pitfalls that arise in chronic care management, data inaccuracy and documentation can impact patients the most. Since most of the care delivery in CCM is backed by data, inaccurate data can lead to inaccurate treatment and diagnosis, ultimately impacting patient health outcomes. The best way to avoid pitfalls related to data is by smooth integration and making the software interoperable.
Along with that, healthcare providers in CCM often struggle with improper documentation. Documentation is a necessary requirement for billing for chronic care management programs. Pitfalls in documentation can lead to delays in reimbursements and can even invite legal troubles, damaging the practice’s reputation.
How to Avoid Common Pitfalls with a Good Team and Powerful Software
The most common pitfalls in CCM are often related to the designated care team and the software. Having a good team can be incompatible if the software is unable to keep up or vice versa.
To avoid such pitfalls and challenges in CCM with a good team, here are a few things that can be considered:

- Education and training: Training the team with the specific requirements of chronic care management and with the CCM software can help in the long run and even contribute to the success of the program.
- Assign Clear Roles and Responsibilities: Defining the roles and responsibilities of each member involved in the program is one of the CCM best practices in the industry. This streamlines most of the process and workflow.
- Clear and Effective Communication: Encourage clear and open communication within the team, and regular meetings can further increase collaboration. This can ensure that everyone is on the same page and working towards the same goal.
To avoid such common pitfalls with powerful software, here are some CCM best practices that can be considered:

- User-friendly Interface: Understand that the care team are not tech experts. Ensure that the software has a user-friendly interface for the team to easily navigate through and reduce the chances of errors.
- Comprehensive Patient Data Management: The software must be capable of managing all aspects of patient data with accuracy and real-time updates in the patient’s medical history, treatment plans, etc.
- Interoperability and Scalability: Ensure that the software can easily allow sharing of patient data with other healthcare systems. Along with that, the software should also be capable and flexible enough to accommodate the growth of the CCM program.
- Security Measure: Patient data is sensitive in nature, and mishandling it can lead to legal troubles. Ensure that the CCM software is HIPAA compliant and abides by the privacy regulations.
User Training: As mentioned earlier, power software is useless if people are unable to use it. Provide effective training to the team to help them understand the software better and how to use it effectively.
Conclusion
A chronic care management program is simple and not tricky only if you understand the program. Also, before starting the program, addressing the pitfalls and challenges in CCM it brings can help easily overcome them. Above are the most common pitfalls healthcare providers face when implementing a CCM program.
So, ask yourself the questions mentioned above and make your chronic care management program successful by avoiding the most common mistakes others commit.
Top 10 Essential Tips for Avoiding Common CCM Pitfalls
Frequently Asked Question’s
Some of the most common pitfalls in CCM program are:
- Enrolling enough patient population
- Getting patient consents
- CCM practices dedicated healthcare staff
- Patient engagement and education
- Implementing CCM software with practice
Here are some of the ways to optimize chronic disease management:
- Instilling patient-centric care approach
- Implementing technology and digital solutions
- Enhancing care communication and coordination
- Promoting healthy lifestyle in patients
- Timely care interventions and care plan adjustments
Below are the best practices that you can implement for effective chronic care management:
- Focusing on patient-centric care
- Leveraging technology and implementing digital solutions
- Fostering better care team communication and coordination
- Understanding patient eligibility
- Comprehensive care plan development
- Knowing CCM billing services
- Accurate time tracking for providing care services
Some of the most common mistakes in CCM that you should avoid in implementation are:
- Lack of planning and strategic implementation
- Poor patient engagement strategies
- Integration and interoperability challenges
- Poor care team communication and coordination
Some of the best practices in CCM to enhance care coordination are:
- Maintaining a good patient-provider relationship
- Integrating EHR, Telehealth, and Clinical decision support system
- Fostering care team collaboration and coordination
CCM metrics like increased patient engagement, timely care interventions, care plan adjustments, patient-provider communication, reduced manual clinical workflow, and improved patient health outcomes can be used to measure the success of chronic care programs.