Did you know that physicians spend almost 20% of their time on desk work?
Understanding Your Needs and Defining Your Budget
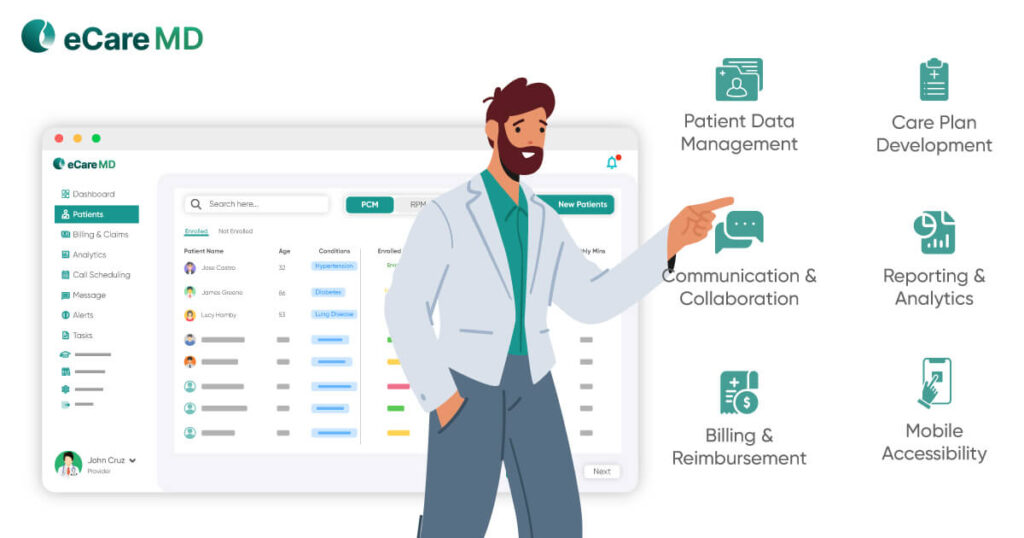
Evaluating Essential Features and Functionality
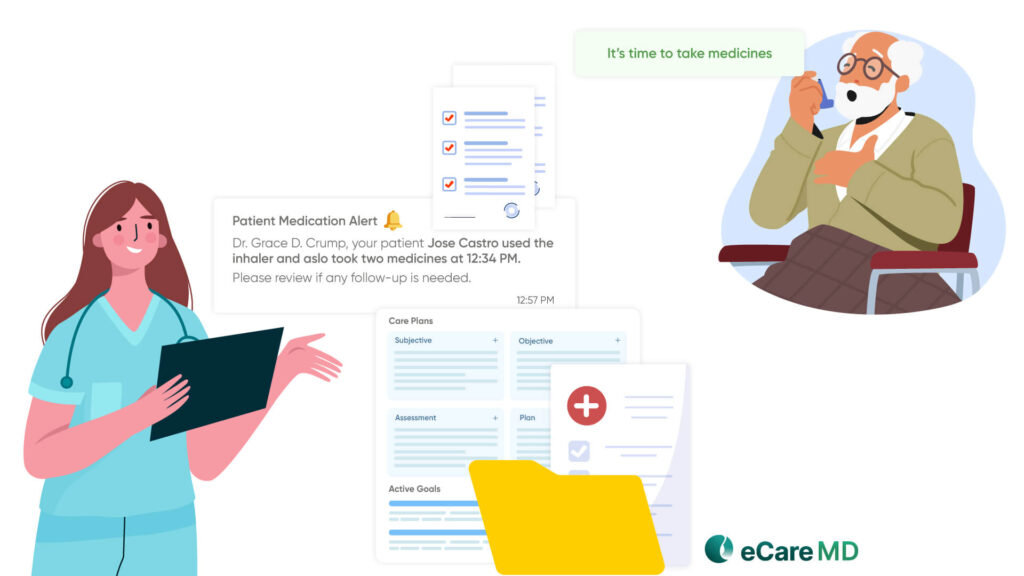
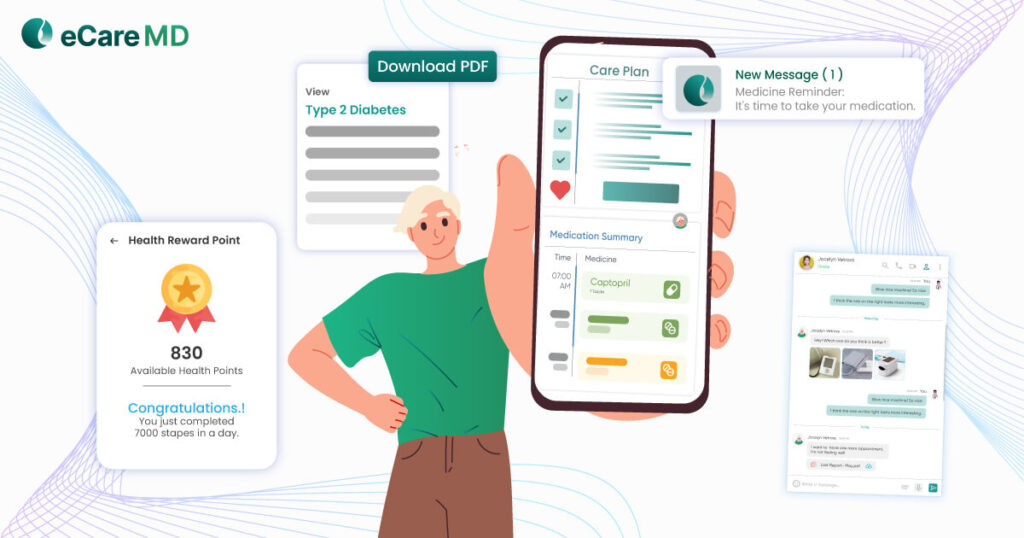
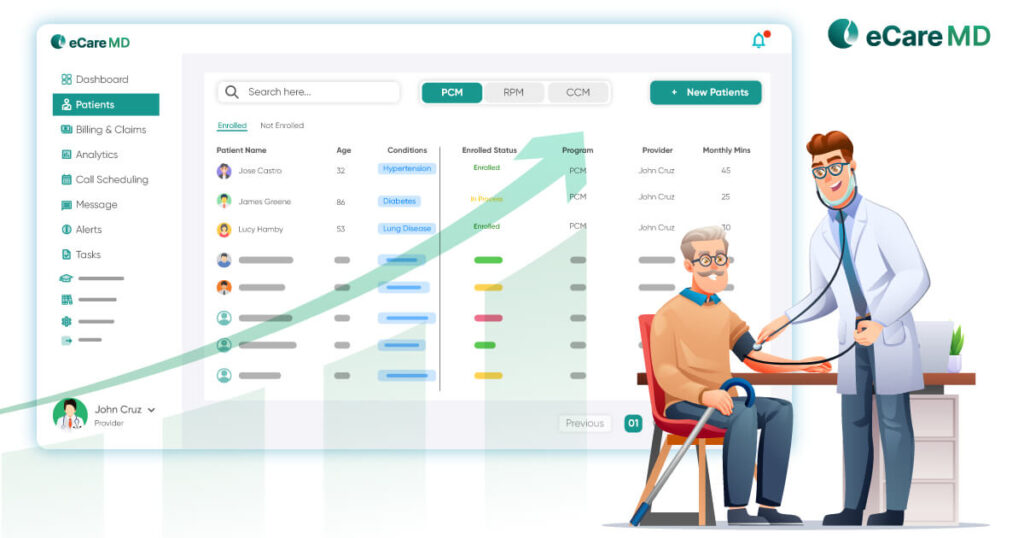
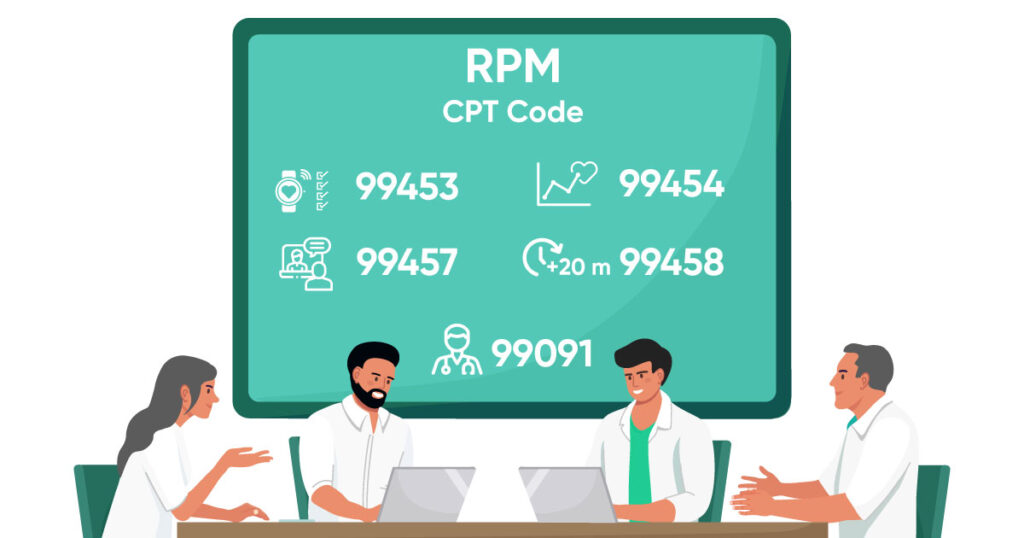
- Patient Tracking and Monitoring: This feature enables real-time documentation of patient interactions, scheduled follow-ups, and ongoing care management activities. Having a track of everything leads to reduced missed follow-ups, enhanced patient engagement, and ensures continuity of care.
- Care Plan Development: Personalized care plans are at the heart of effective chronic disease management. With a care plan development feature, providers can create, update, and track patient-specific treatment strategies tailored to their condition. Implementing this feature improves patient adherence, enhances care coordination, and optimizes treatment outcomes.
- Automated Reporting and Documentation: Documentation is one of the most time-consuming processes in any care practice, but it is essential for billing, reporting, and many other things. But, when you automate this process, it reduces, if not eliminates the need for manual entries and saves time for healthcare providers. It also brings benefits like increased billing accuracy and helps maximize reimbursements.
PCM Software Evaluation Checklist
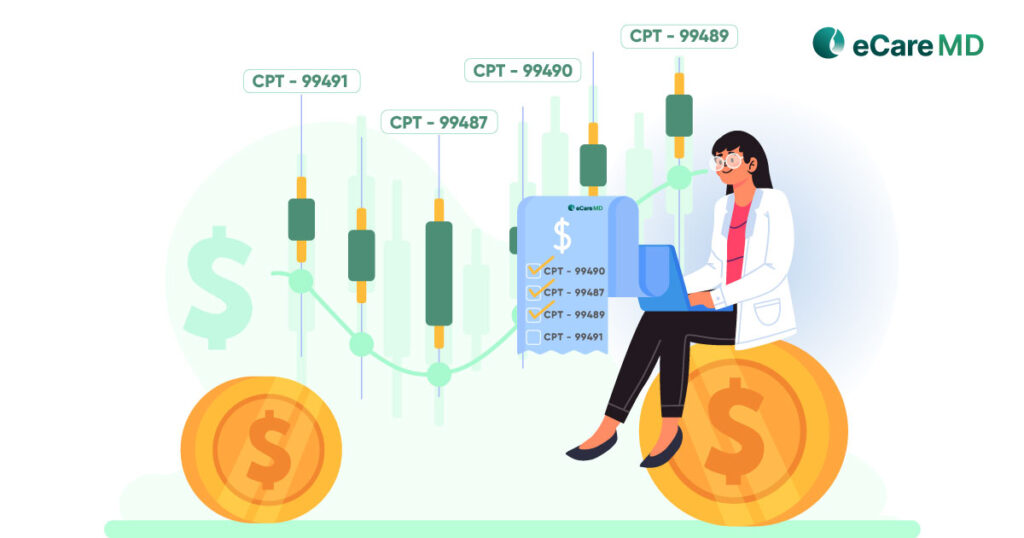
Download Free ChecklistComparing Pricing Models and Identifying Hidden Costs
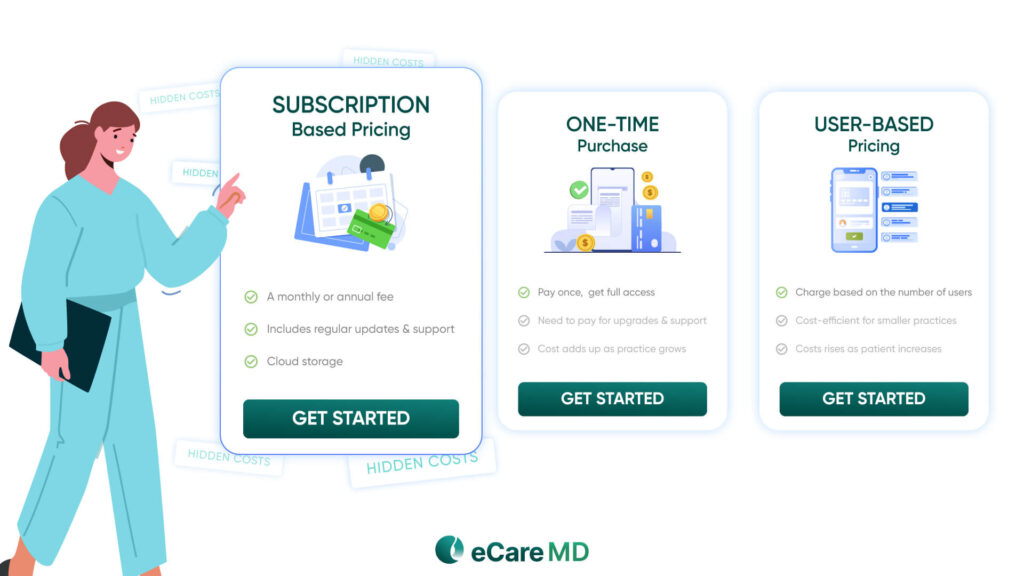
- Subscription-Based Pricing (SaaS): A monthly or annual fee is required for continued access to the software. The plus point of this model is that it often includes regular updates, support, and cloud storage, making it a predictable expense. However, the costs can rise as your practice grows and you require additional features and more cloud storage.
- One-Time Purchase: In this, you only have to pay once, and you get full access and ownership of the software. While this avoids recurring fees, you may still need to pay for upgrades, support, and additional features separately. This makes it expensive in the long run, and the cost adds up as your practice grows.
- User-Based Pricing: Some vendors charge based on the number of users, patients enrolled, or PCM-related claims processed. This can be cost-efficient for smaller practices but expensive as patient volume increases.
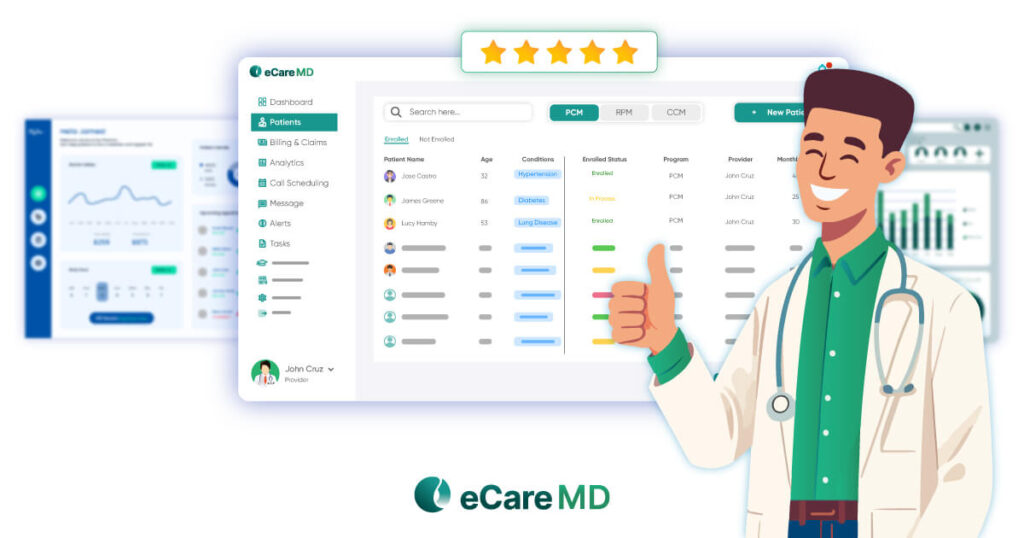
Prioritizing Vendor Reputation and Customer Support
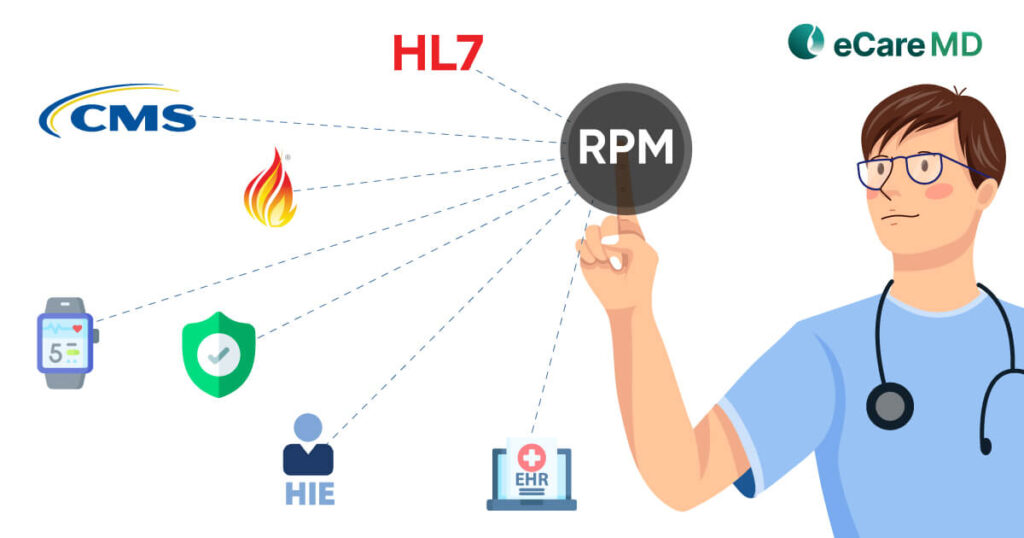
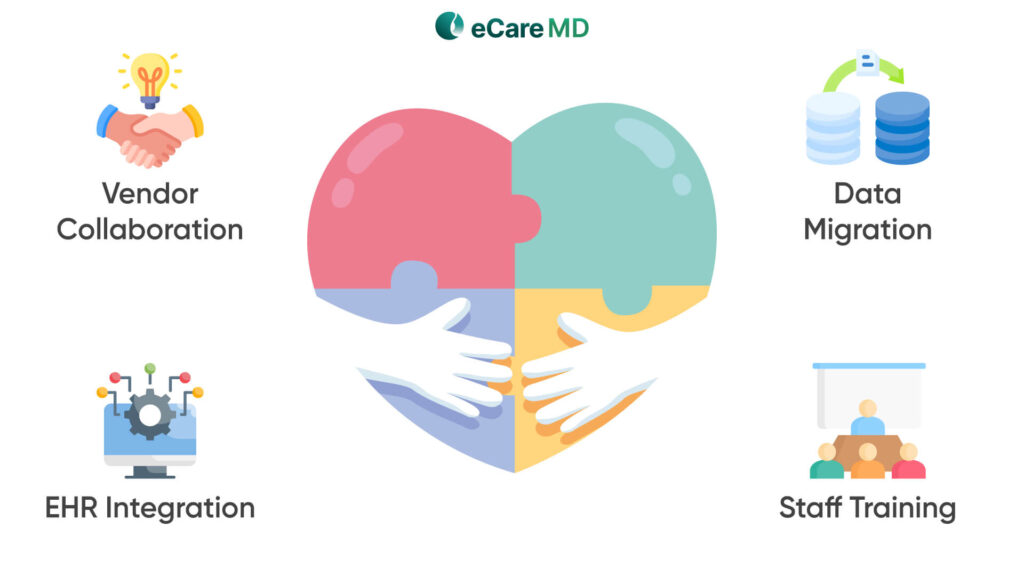
Streamlining Implementation and Ensuring Seamless Integration
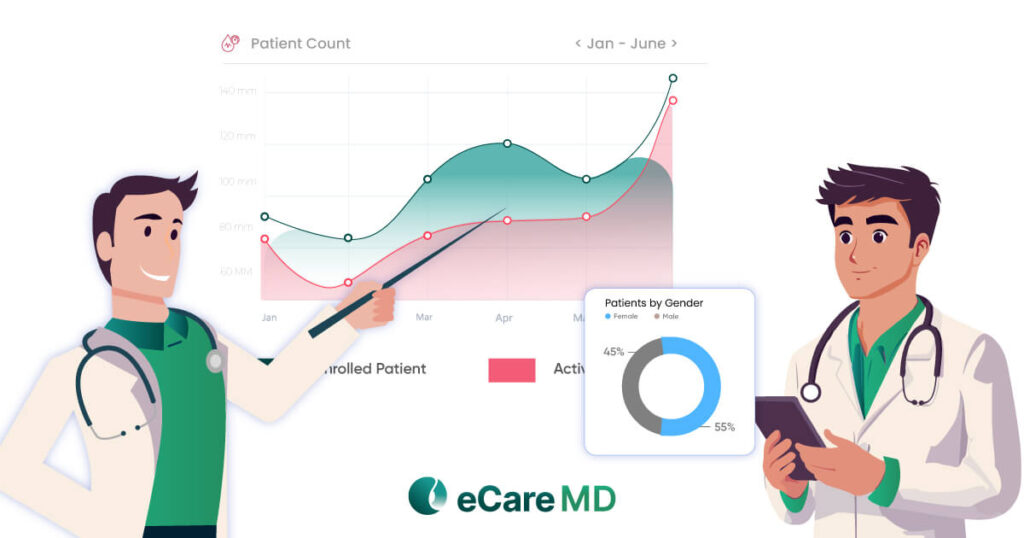
Maximizing ROI and Measuring Success
Furthermore, you have to evaluate the software and workflows to identify the gaps and then optimize them accordingly. In this, taking staff and patient feedback can prove to be important and provide you with needed insights. In short, by continuously measuring the success and refining your processes, you can achieve maximum principal care management ROI, enhance patient care and ensure long-term growth with PCM software.
Conclusion
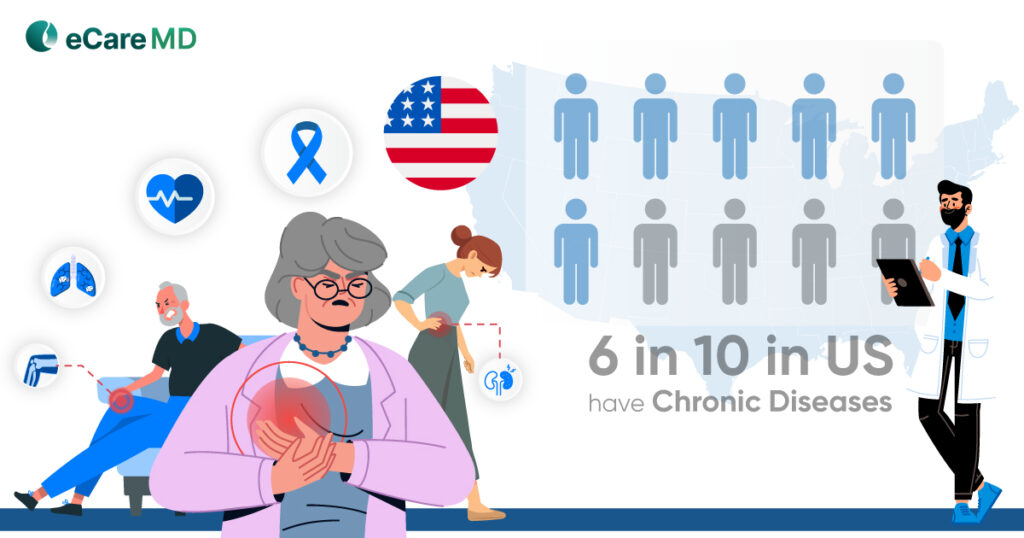
When choosing cost-effective principal care management (PCM) software, you must consider some factors. First, choose software that will have all the core features, such as patient tracking, automated reporting, and care plan development.
However, while doing so, also pay attention to the hidden costs, implementation costs, and ownership costs. When you are finalizing the software, ensure that you check if it is subscription-based or one-time purchase software. Each software’s features and functionalities will vary, as will the cost. So, choosing software that will be cost-effective for you is crucial.
Are you unsure which software is right for you? Let us help! Click here to schedule a free demo with eCareMD and discover an affordable, efficient PCM solution tailored to your needs.