Did you know around 133 million people suffer from chronic conditions in the United States alone?
The mounting pressure of providing care to chronically ill patients has been immense and a costly affair for both patients and providers. To reduce the burden and overall healthcare costs and improve healthcare practices, the Center for Medicare and Medicaid Services (CMS), in 2015, introduced the Chronic Care Management Program. It included specific CPT codes and set the ground rules to bill for the service healthcare providers are providing.
CPT Codes for chronic care management give providers a brief idea about billing opportunities, criteria, timeframe, and standards. This simplifies the reimbursement and billing cycle for clinical practices, improving overall productivity.
In this blog, we will discuss everything about chronic care management billing, including CPT codes for chronic care management, billing for chronic care and chronic care management reimbursement procedures.
Key Requirements for Billing the Chronic Care Management (CCM) CPT Codes
According to CMS, there are certain requirements that need to be met by the providers for each chronic care management reimbursement. Below are the following requirements:
1. Billing Practitioner
As per the guidelines set by CMS, the chronic care management billing practitioner must be a certified physician, certified Nurse Midwife (CNM), Nurse Practitioner (NP), or Physician’s Assistant (PA), and one practitioner can only bill or reimburse for the CCM program for one patient in one month.
Along with that, the billing practitioner can only bill the patient for either complex CCM (CPT codes 99487/99489) or non-complex CCM (CPT codes 99490/99439 or CPT codes 99491/99437) in one calendar month.
2. Patient Eligibility
CMS has also set the eligibility criteria for patients who can opt for the CCM program:
- The chronic care management program can be availed by patients who have at least two chronic conditions, which are predicted to last at least a year or a lifetime. Apart from that, the severity of the condition is also taken into account.
- In case the care plan is unchanged or only has a minimal change, then the complex CCM cannot be billed.
3. Consent
To be a part of the chronic care management program, written or verbal consent from the patient is required. Along with that, it is the duty of the practitioner to inform the patient about the services included in chronic care management and the cost-sharing options.
4. Initiation Via Face-to-Face Visit
To initiate the chronic care management program for a new patient, an initial face-to-face visit with the billing practitioner is required. However, the initiating visit must not be part of the CCM program and cannot be billed for the same. This initiating visit can be a part of an Annual Wellness Visit, an Initial Preventive Examination, or even a Level 2-5 E/M visit.
5. Minimum Time Requirements
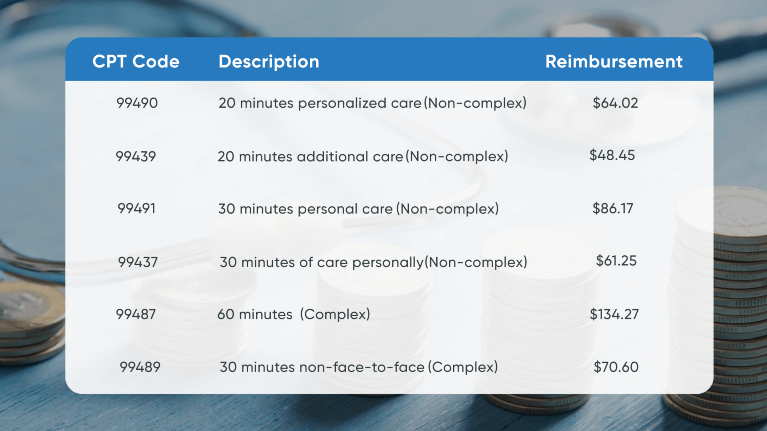
For every chronic care management reimbursement, CMS has set a minimum time requirement for every service provided for chronic care management billing. Below are the minimum time requirements for each CCM CPT code:
Non Complex CCM
- CPT Code 99490 – Minimum 20 minutes of non-face-to-face monitoring of the patient in a calendar month.
- CPT Code 99439 – Minimum 20 minutes spent by clinical staff in providing CCM services.
- CPT Code 99491 – Can be billed once a month with a minimum of 30 minutes spent by a physician or non-physician practitioner on providing CCM services.
- CPT Code 99437 – Additional 30 minutes of chronic care management services provided by a physician or non-physician practitioner, typically billed in conjunction with CPT Code 99491.
Complex CCM
- CPT Code 99487 – Minimum 60 minutes of non-face-to-face consultation for complex CCM service in a calendar month.
- CPT Code 99489 – Additional 30 minutes of non-face-to-face consultation services provided in a calendar month, billed in conjunction with CPT Code 99487.
6. Duplicative Concurrent Billing
Chronic care management billing for one particular patient can be billed by only one provider or clinician in one calendar month. The billing practitioner cannot bill complex CCM and non-complex CCM services in the same calendar month. Along with that, CPT codes 99490/99439 and CPT codes 99491/99437 cannot be billed in the same calendar month.
Some additional chronic care management reimbursement guidelines set by CMS do not allow the billing practitioner to bill complex CCM codes with prolonged E/M (Evaluation and Management) Services.
Proven CCM Billing Strategies
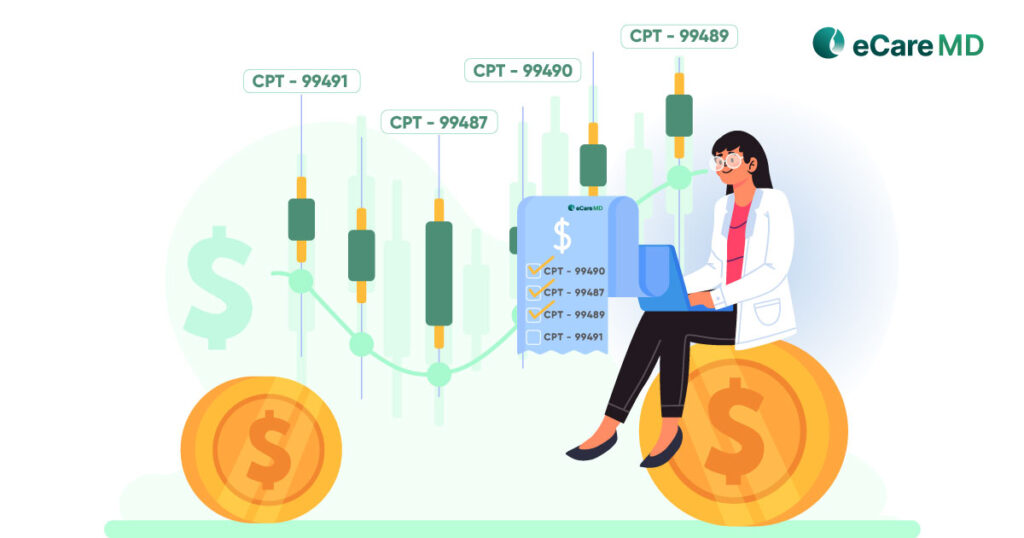
CPT Codes for Chronic Care Management
1. CPT Code 99490: Non-complex Chronic Care Management Service
Under the CPT 99490, the provider is allowed to reimburse the amount for providing non-face-to-face monitoring on non-complex chronic care management. Usually, this is provided by the clinical staff or care coordinator under the supervision of a physician.
The main focus of this code is to provide preventive care to the patient, and to qualify for CPT 99490, a minimum of 20 minutes of personalized care is required. The amount reimbursed with this code is $64.02 on average for last year.
2. CPT Code 99439: Non-complex Chronic Care Management Service
CPT 99439 is used as a follow-up code for CPT 99430, where additional care for 20 minutes is provided for non-complex chronic care management.
This code is to be used when the clinical staff provides additional consultation when the initial time allowed under CPT 99490 is consumed. The amount reimbursed with this code is $48.45 on average for last year.
3. CPT Code 99491: Non-complex Chronic Care Management Service (Physician)
CPT 99491 is used to reimburse a minimum of 30 minutes of care personally provided by physicians or non-physician practitioners. This is an add-on code to CPT 99490 and has similar patient eligibility criteria.
This code focuses on establishing comprehensive care, and the amount reimbursed with this code is $86.17 on average for last year.
4. CPT Code 99437: Non-complex Chronic Care Management Service (Physician)
CPT 99437 is used to reimburse subsequent 30 minutes of care personally provided by physician or non-physician practitioners. This is an add-on code to CPT 99491 and covers the additional time for providing care covered by CPT 99491.
The amount reimbursed with this code is $61.25 on average for last year.
5. CPT Code 99487: Complex Chronic Care Management Service
Under CPT 99487, the provider is allowed to reimburse the amount for providing non-face-to-face consultation for complex patients for a minimum of 60 minutes. It was introduced in 2017 and is usually carried out by clinical staff.
Other than the usual requirements, to qualify for this, the chronic condition of the patient must have a high risk of death, functional decline, or decompensation. The amount reimbursed with this code is $134.27 on average for last year.
6. CPT Code 99489: Complex Chronic Care Management Service
CPT 99489 is to be billed with CPT 99487 for every additional 30 minutes of non-face-to-face consultation provided. The amount reimbursed with this code is $70.60 on average for last year.
Impact of CCM on Revenue Cycle
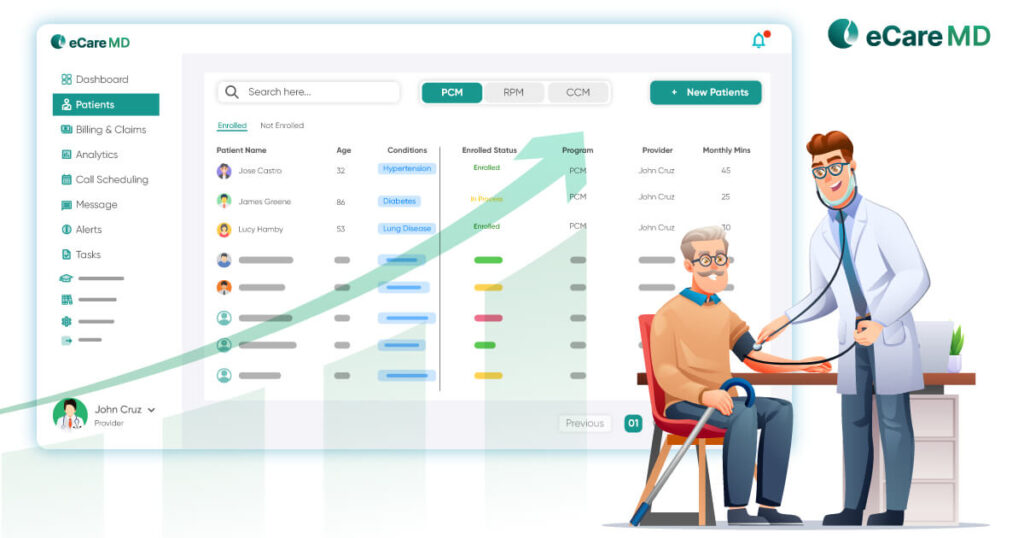
Chronic care management programs have been introduced to reduce the burden on healthcare providers and increase revenue for healthcare providers by reducing overall healthcare costs. By incorporating a CCM program, clinics can have a new source of revenue with an additional $85000 per year per billing provider. Though there is no assurance of earning the said amount from the program, if implemented correctly, it can surely increase the revenue for the clinical practices.
Another impact the CCM program has on practices is to reduce the chances of hospital readmission and emergency visits and reduce nursing costs. Again, this helps healthcare providers improve the efficiency of their care practices and reduce staff costs.
Furthermore, CCM programs ensure that the providers are paid for the services they provide. Some of the components to look for this are identifying patient eligibility, accurate documentation and billing, and timely follow-ups. To effectively manage the revenue cycle, providers can always opt for RCM (Revenue Cycle Management) to ensure timely reimbursements.
Conclusion
A chronic care management program was introduced in 2015 to help patients reduce the overall costs associated with chronic care. Furthermore, it also provided clinics with a new source of revenue while reducing the burden on healthcare providers.
Chronic care management software can help healthcare providers ensure accurate billing and receive timely reimbursements for the services they provide. Chronic care management software can not only assist providers in the creation of care plans and streamline clinical workflow but also simply bill and encourage accuracy in patient care.
Frequently Asked Question’s
Below are the CPT Codes used for the chronic care management program in 2024:
- CPT Code 99490
- CPT Code 99439
- CPT Code 99487
- CPT Code 99489
- CPT Code 99491
- CPT Code 99437
The major difference between complex and non-complex CCM CPT Codes is the complexity of the chronic condition the patient is suffering from. These codes indicate the level of care the patient is receiving through the program.
The time required to qualify for each CCM CPT Code is different. For example, CPT Codes 99490 require a minimum of 20 minutes of care managers and 99491 require minimum 30 minutes of physician, whereas CPT Codes 99487 require a minimum of 60 minutes. The other CPT Codes, 99439 and 99489, are add-on codes for CPT Codes 99490 and 99487, respectively. Going through the CMS CCM CPT Codes guidelines is necessary for clarification.
The documentation required for submitting CCM claims are:
- Patient consent
- Clinical notes
- Progress notes
- Patient communication logs
- Care Plan Reports
- List of chronic conditions
- Time Logs
- Billing report mentioning eligible CPT codes for logged time with service provided
Typically, CMS covers 80% of the reimbursements for CCM services under Medicare Part B. The rest of the 20% is covered through a co-pay or patient. However, depending on the insurance, the payers can, and charges can vary.
Each CCM CPT Code has different reimbursement rates. The average for CPT Codes 99487 and 99490 are $135 and $64, respectively. The reimbursement rate for other follow-up codes is less than the major CPT Codes.
The potential denials for CCM claims are often related to improper billing. Some of the chronic care management best practices to avoid denials are:
- Specific claims
- Verifying eligibility and claims
- Accurate time logs
- Timely claim submission
- Accuracy in billing
Yes, you need to get the patient’s consent to provide CCM services to your patients. However, the consent can either be in written or verbal.
The CPT Codes used for the chronic care management program in 2024 are:
- CPT Code 99490
- CPT Code 99439
- CPT Code 99487
- CPT Code 99489
- CPT Code 99491
Each CCM CPT code has a different reimbursement rate. Below are the national average rates for each CPT Code:
- CPT Code 99490 – $64.02
- CPT Code 99439 – $48.45
- CPT Code 99487 – $135.27
- CPT Code 99489 – $70.25
- CPT Code 99491 – $86.17
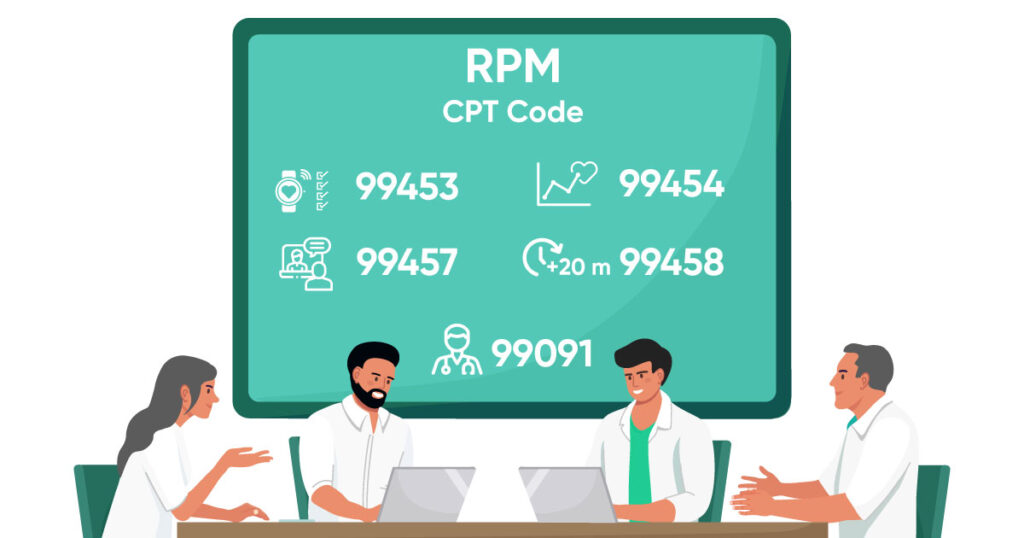
Yes, since the CCM program requires RPM, the provider can bill for both CCM and remote patient monitoring.