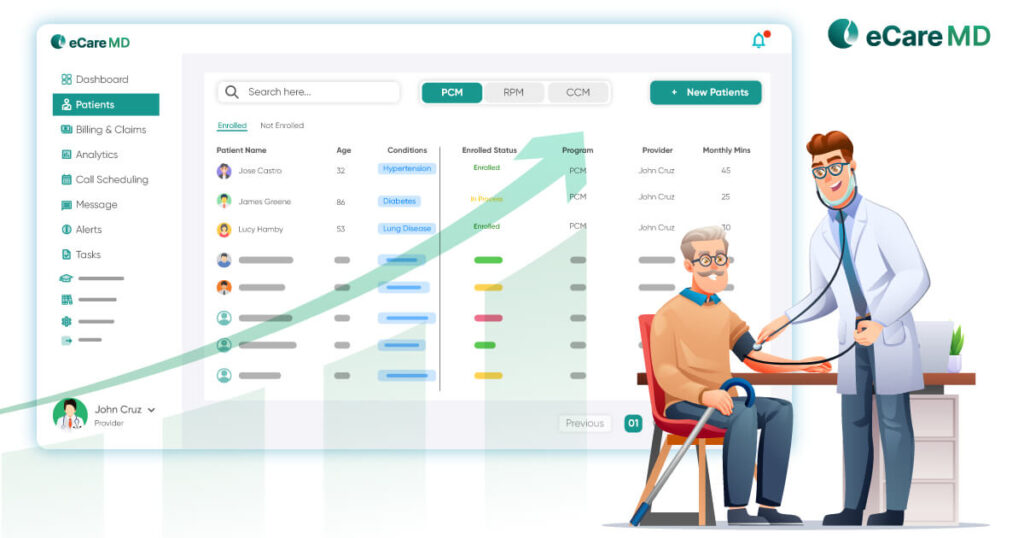
Did you know that 65% of doctors use RPM to manage patients’ medical conditions?
Given the rising adoption rate of remote patient monitoring, medical institutions across the world are adopting the RPM program. However, the lucrative use of remote patient monitoring offers a unique opportunity to add an additional source of income; around 24% of claims denials are observed in a doctor’s first initial consultation.
That is the reason some of the clinicians are still skeptical about starting their own remote patient monitoring program. RPM claims processing involves coding, documentation and other necessary things to ensure proper reimbursement.
So, here are the eight things that must be known for proper billing and claims in remote patient monitoring programs.
Understanding Eligibility Criteria

Grasping Covered Services
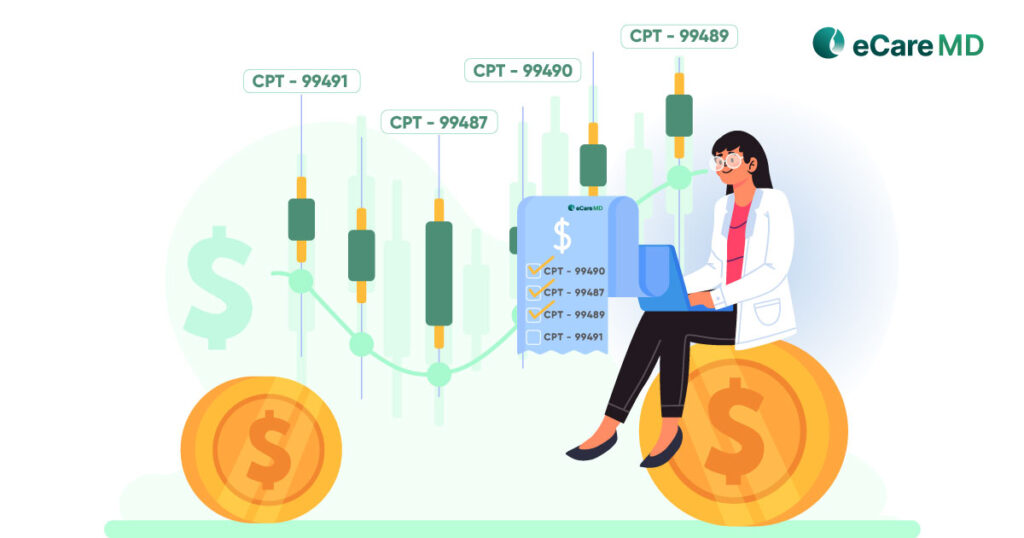
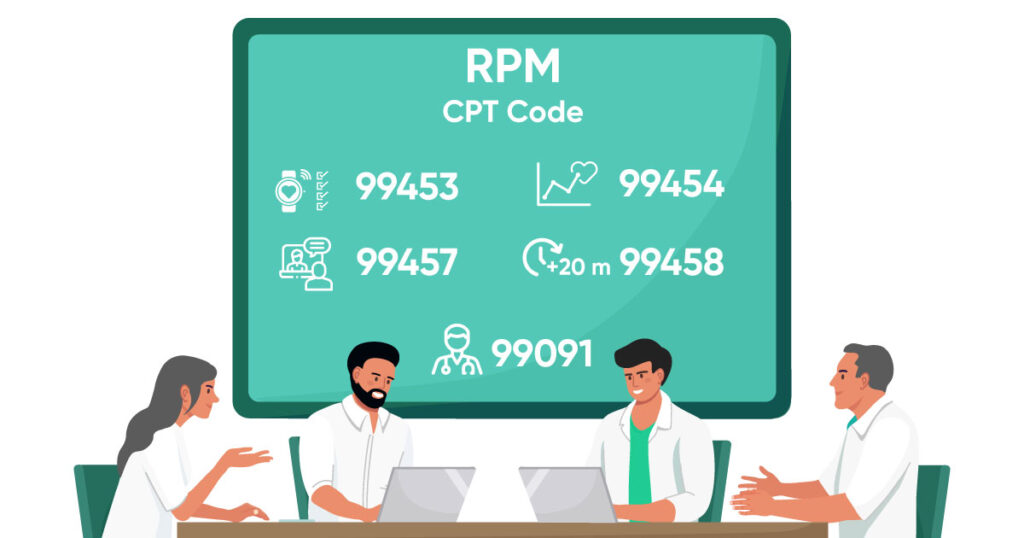
Mastering CPT Coding
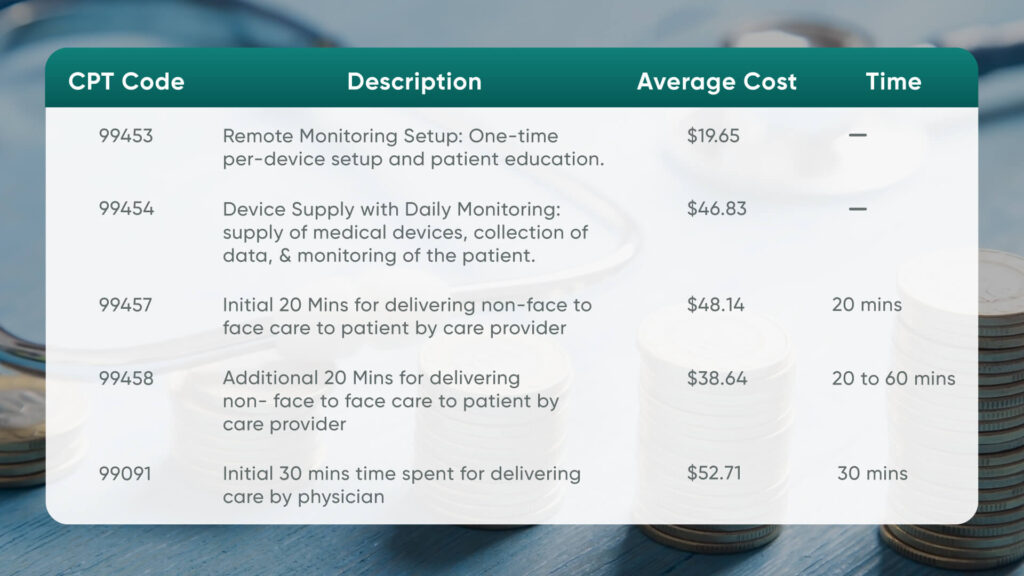
- CPT Code 99453: Covers RPM device set-up and patient education on device usage.
- CPT Code 99454: Covers the supply of devices for daily recording and programmed alert transmissions.
- CPT Code 99457: Covers initial 20 minutes of treatment by clinical staff over 30 days.
- CPT Code 99458: Covers an additional 20 to 60 minutes of reimbursement in a calendar month.
- CPT Code 99091: This new CPT code, introduced in 2022, covers a minimum of 30 minutes of care, medical management, and monitoring advising.
Building a Strong Care Plan
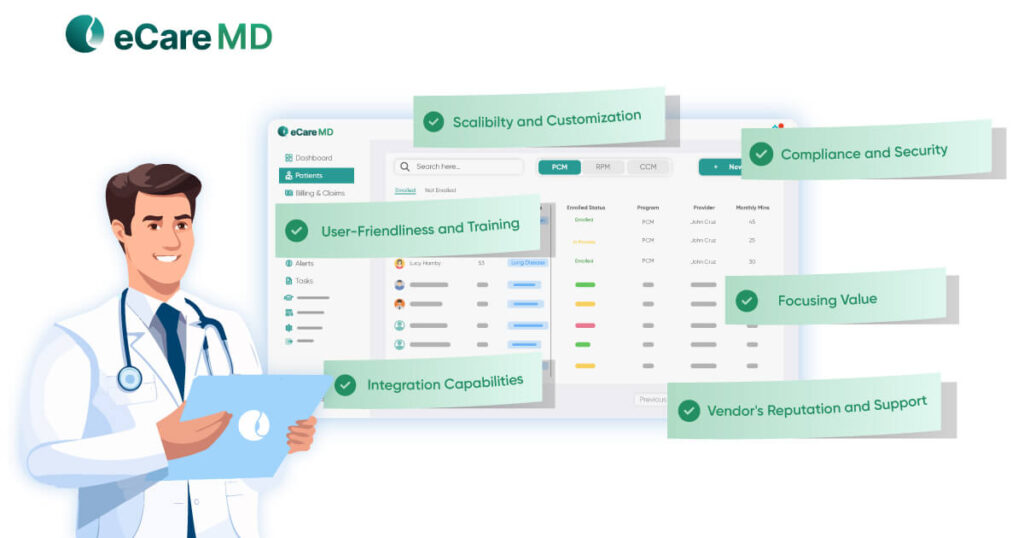
Partnering with Coders
Streamlining Claims Submission
Staying Updated on Regulations
To stay updated with these regulations, consulting reliable sources like its official website is suggested. Otherwise, you can refer to a professional association for the latest updates.
Addressing Potential Audits
As a healthcare entrepreneur, you must know that payers also conduct audits every once in a while. Healthcare providers who have started remote patient monitoring programs have to rely heavily on appeals for denied RPM claims after payer audits. That is why it is advised to maintain detailed records and documentation to instill best practices in your RPM billing practice. This will not only help you streamline the process but act as a preparation for any audits conducted by payers.
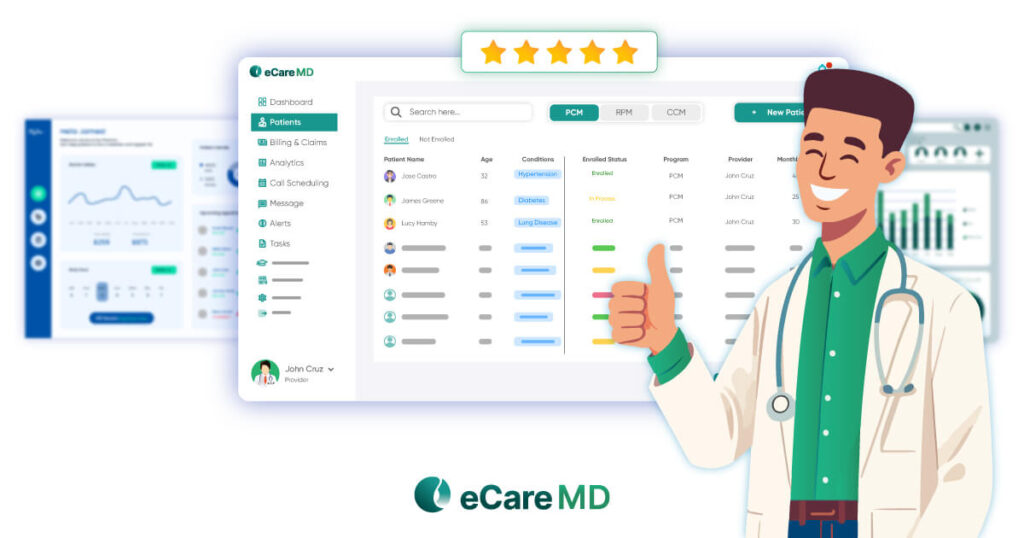
Conclusion
To streamline your billing and claims process, it is important to cover all the essential things, from understanding the eligibility criteria to CPT codes and their usage. Let this blog be your guide to instilling a robust billing and claims process.
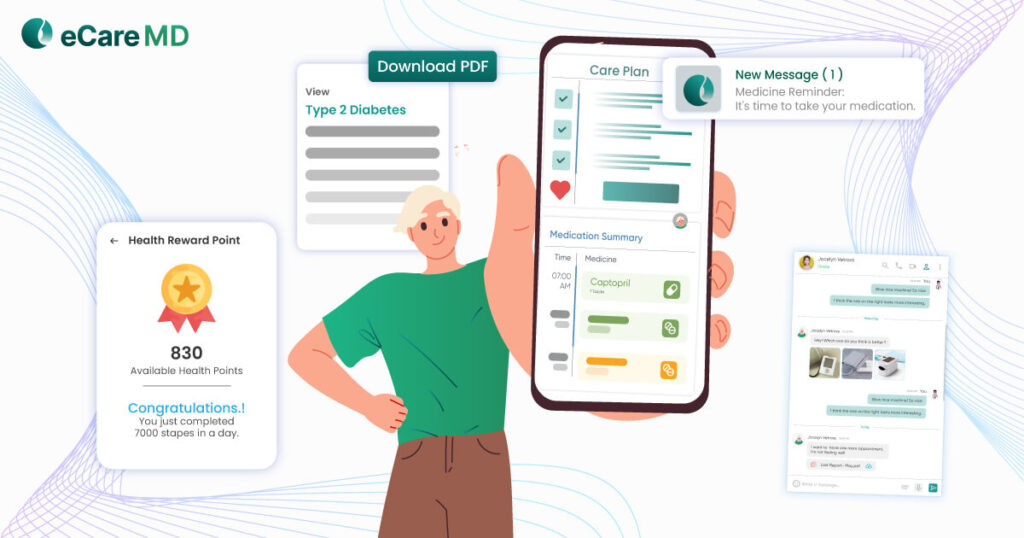
Furthermore, to make the billing process and claims transparent, patients should be proactively engaged in their care practices and informed about everything. Encourage patients to have ongoing communications with healthcare providers, which will help improve patient outcomes and make your RPM program a success.
Frequently Asked Question’s
Choosing the right code for billing RPM services can feel technical, but it’s like picking the perfect key for a lock. Here’s a simpler way to think about it:
- Setting things up: If you’re starting the program and providing equipment, use code 99453. Think of it as the key that unlocks the patient’s remote monitoring journey (as long as data is collected for at least 16 days that month).
- Monthly check-ins: Code 99457 is like your initial 20-minute conversation with the patient about their monitored data. You might also use code 99454 if daily readings are received.
- Extra time needed: If the conversation goes beyond 20 minutes, code 99458 acts like additional keys, each representing another 20-minute chunk.
- Setting things up: If you’re starting the program and providing equipment, use code 99453. Think of it as the key that unlocks the patient’s remote monitoring journey (as long as data is collected for at least 16 days that month).
Remember, this is a simplified explanation. For complete accuracy, consult a medical billing expert or refer to official CPT resources.
Successful RPM claim processing hinges on proper documentation. Key elements include:
- Informed patient consent: Document consent for receiving RPM services.
- Medical necessity: Justify the need for remote monitoring (condition, goals).
- Device details: Specify device type, deployment date, and patient training details.
- Daily data collection: Ensure recordings and review of patient-reported data.
- Regular review and action: Document analysis of readings and any actions taken based on results.
Detailed records strengthen your claim and ensure proper reimbursement.
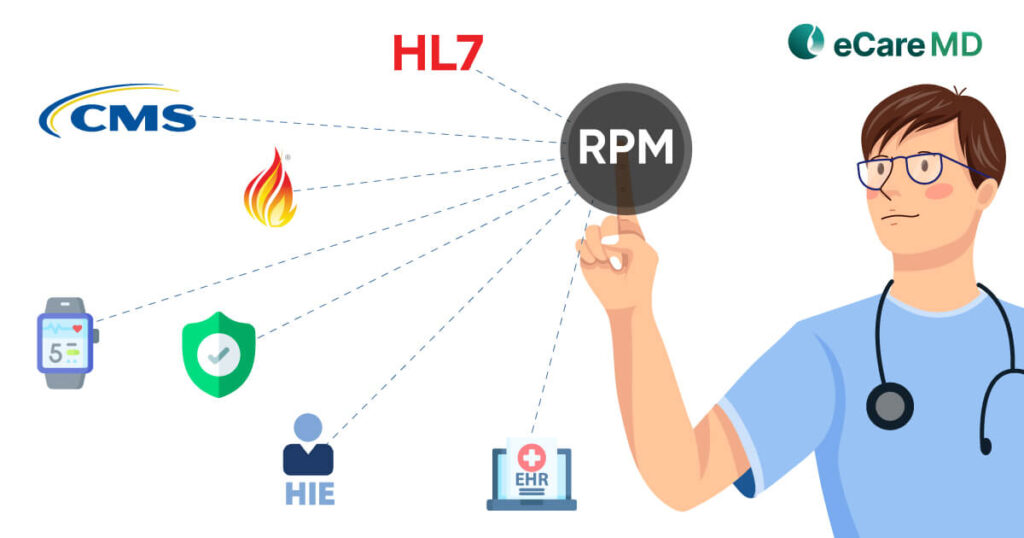
HIPAA safeguards patient data in RPM programs. Here’s the gist:
- Secure technology: Ensure data encryption (both storage and transit) by the RPM vendor.
- BAA: Establish a Business Associate Agreement with the vendor outlining data security responsibilities.
- Authorization: Obtain written patient consent for data collection and sharing.
- Internal controls: Implement staff training, data access restrictions, and breach response protocols.
A denied RPM claim requires investigation. Here’s a simplified approach:
- Understand the reason: Review the Explanation of Benefits (EOB) for denial details. Common reasons include missing pre-authorization, incorrect coding, or insufficient medical necessity documentation.
- Verify requirements: Ensure you met all criteria for RPM billing as per your insurance carrier’s guidelines.
- Appeal for denied RPM claim: If valid reasons exist, gather supporting documents (e.g., clinical notes) and submit an appeal following the insurance provider’s process.
Consider consulting your billing department or a healthcare attorney for further assistance with the appeal process.
Reimbursement for RPM services isn’t immediate. Here’s a simplified view:
- Claim submission: Submit claims after the 30-day monitoring period with at least 16 days of collected data.
- Processing time: Insurance companies typically process claims within 30-45 days.
- Payment: Once approved, expect payment within another 15-30 days.
The entire process can take 60-90 days on average.
Billing for additional RPM services beyond monthly monitoring involves identifying time spent exceeding the base coverage.
- Track time providing extra service (e.g., interpreting complex data).
- If exceeding the initial 20 minutes (covered by 99457), use add-on code 99458.
- Bill in 20-minute increments (one code per 20 minutes).
Seek specific guidance from a medical billing professional for accurate coding and claim submission.