Overlooking Integration Capabilities
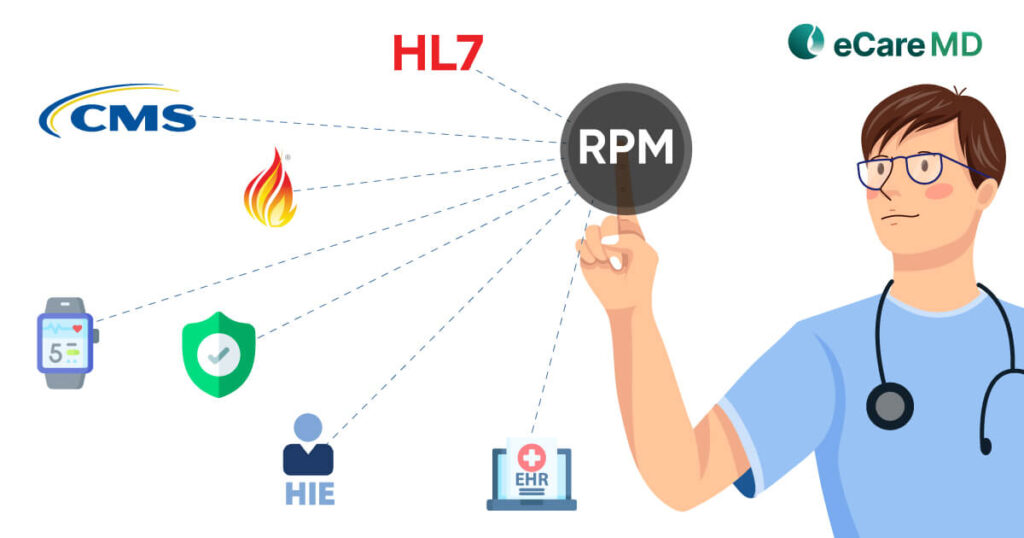
One of the major pitfalls when choosing PCM software is failing to ensure that it integrates seamlessly with your existing Electronic Health Records (EHR). Poorly integrated software leads to inefficiencies, increased administrative burdens, and ultimately compromises patient care. Moreover, when your software fails to integrate with it, data isolation and workflow disruptions are brought about. This may cause your staff to do the data transfer manually, leading to errors, a waste of time, and frustration.
Additionally, with integration, providers forget to check for interoperability with other software, such as telehealth platforms and remote patient monitoring devices. Not having smooth interoperability means your care coordination will suffer in the future, resulting in low patient outcomes.
Furthermore, with time, your practice will grow, and your software will need to grow as well; this is where API (Application Programming Interface) comes in. However, this is also ignored, and in the future, new features cannot be added easily, and you lose the flexibility needed to expand and grow your software and healthcare practice.
Finally, reimbursements are the most crucial aspect of the PCM program, and if your software fails to integrate with billing software, then this process suffers. Without the integration, tracking claims becomes a hassle, leading to potential revenue loss.
So, when you avoid principal care management pitfalls of integration and interoperability, you can streamline multiple aspects of care delivery and improve your revenue.
Ignoring User-Friendliness and Training
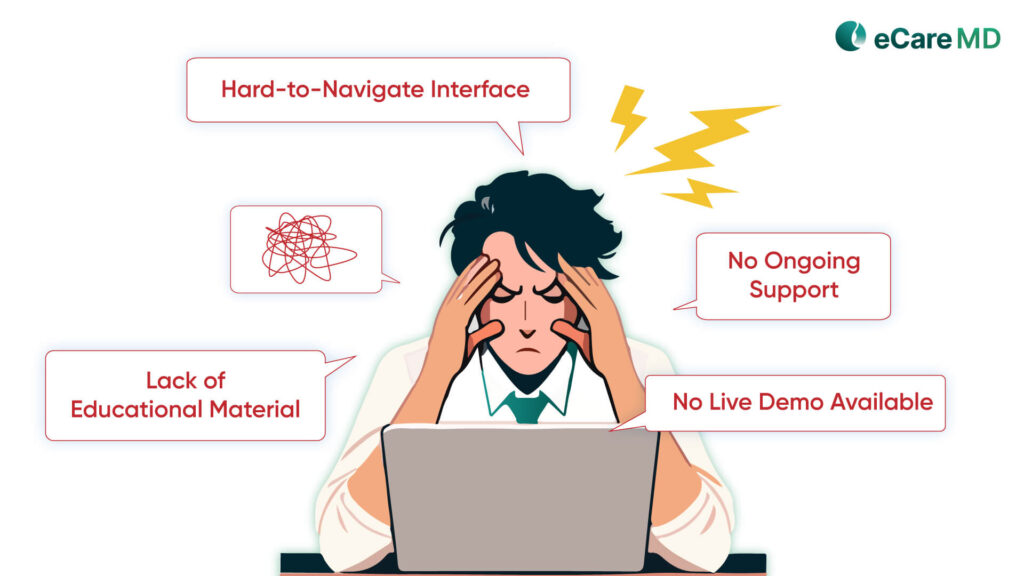
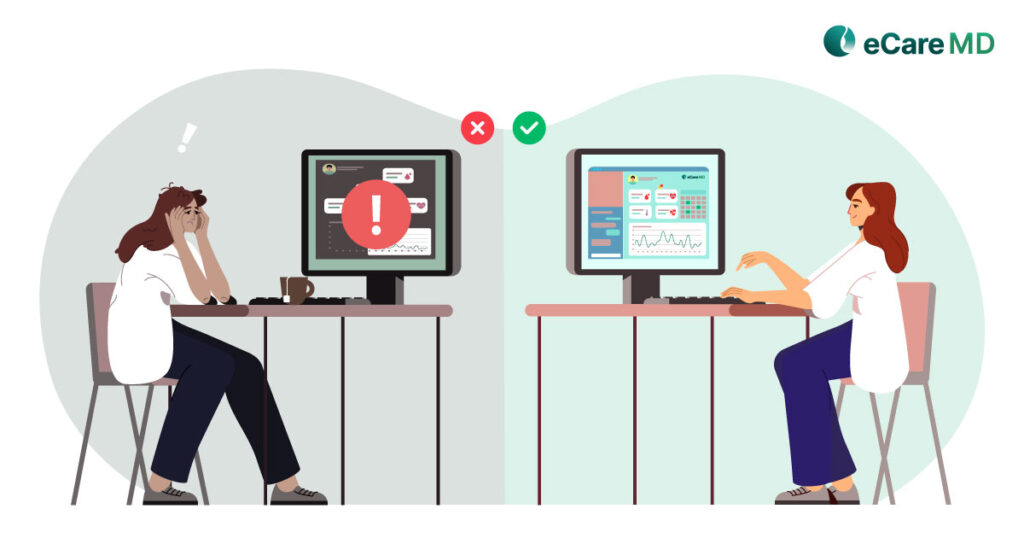
With any software, its adoption is dependent on how easy and user-friendly it is to use. However, many providers who want to cut the cost of software ignore this and buy software with a complex and hard-to-navigate interface. This results in low adoption rates among patients and providers.
In addition, the providers fail to assess the availability and quality of the educational material at the vendor. This lack of educational material leads to difficulty in learning the software functionalities effectively. Also, another mistake that providers make is not inquiring about ongoing support, which leads to more extended downtimes in case of software failure.
Moreover, overlooking mobile accessibility, with the mHealth apps on the rise, becomes quite a big pitfall. It limits the accessibility of providers and patients to quite a large extent and makes providing care on the go difficult.
The reason for this is that it does not ask for a live demo of the software; a live demo helps you understand the software better. This lets you experience the software utility firsthand, ensuring it aligns with your team’s needs before you purchase it.
Neglecting Compliance and Security
If we talk about the biggest and costliest pitfall that providers should avoid, it will be neglecting compliance and security. As the software stores and transmits sensitive patient information, overlooking compliance like HIPAA and GDPR can lead to severe consequences. This can lead to costly fines and reputational damage if there is a data breach and no security measures in place.
Additionally, you should verify that the software is HIPAA certified and that data encryption, along with other data security measures, are implemented. Failing to do so means you are compromising data security. Another common mistake is not considering the software’s ability to track and audit user activity. This ability is necessary for the software to be compliant with the healthcare industry rules and regulations.
Ignoring or not asking for the Business Associate Agreement (BAA) means that in the case of a data breach, you are the only responsible party. This agreement is important because it binds the vendor to protect the patient data and not share it with third parties.
HIPAA Compliance Checklist for PCM Software
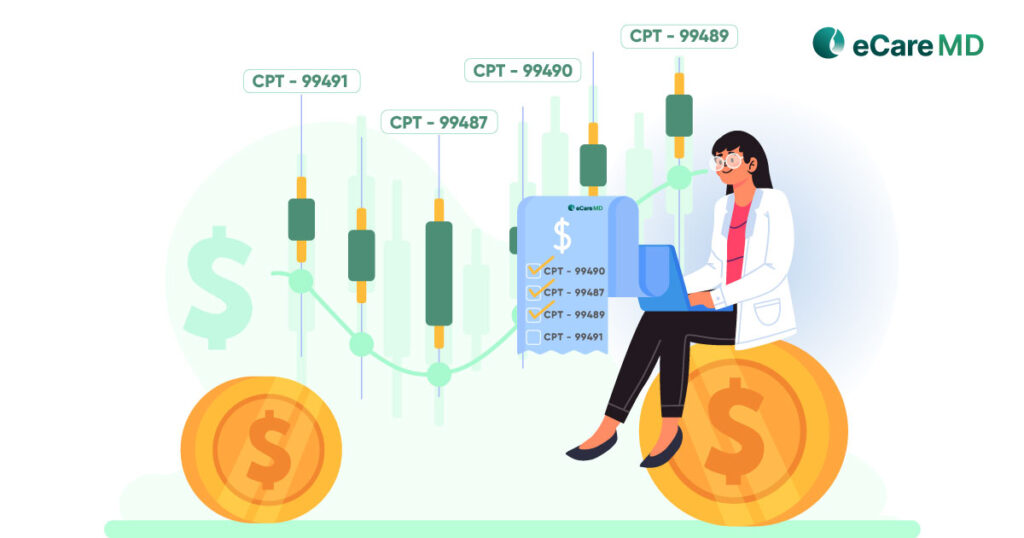
Download For FreeFocusing Solely on Cost, Not Value
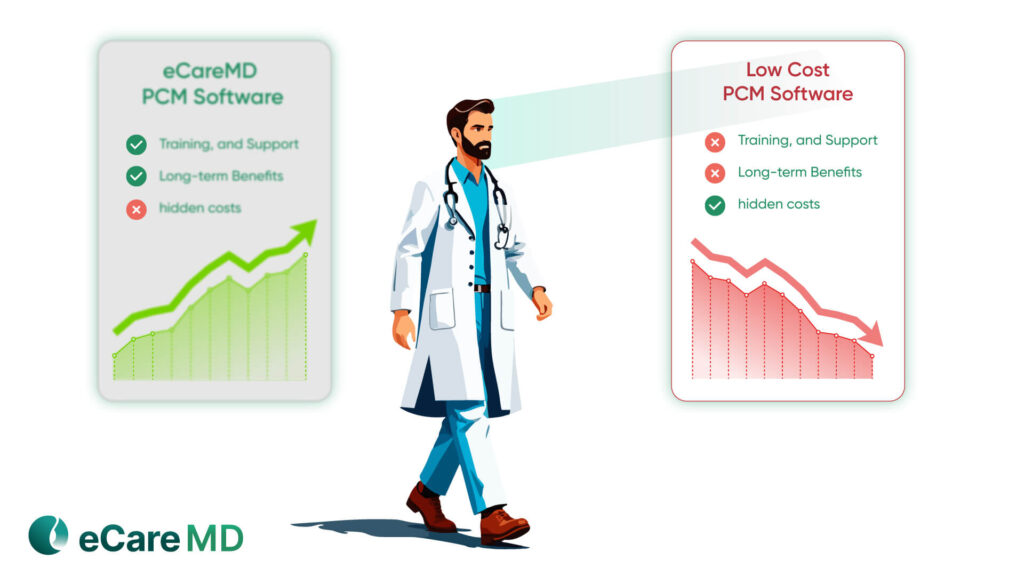
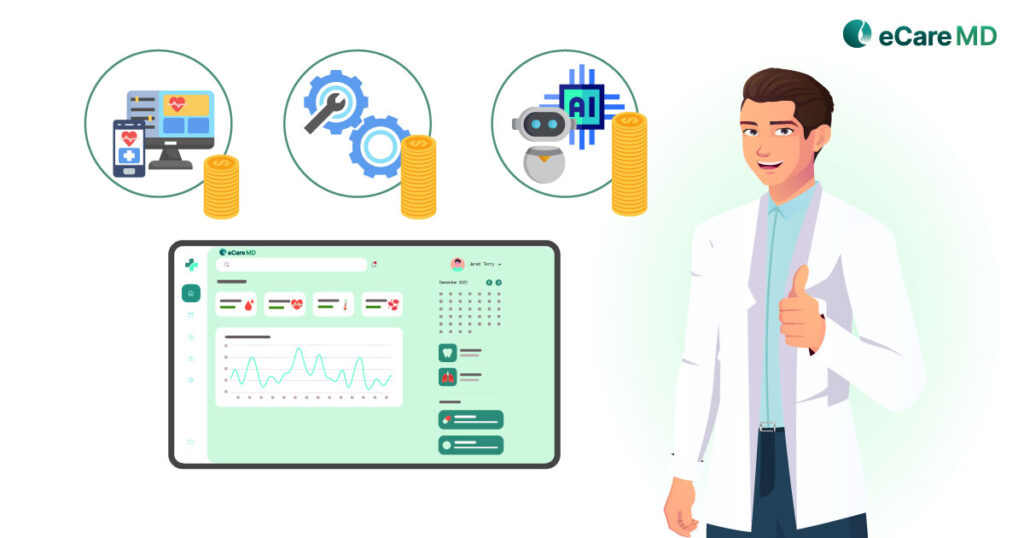
When it comes to choosing cost over value, providers make mistakes by choosing the cost and neglecting the essential features of the software. This lowers the cost of the software, but in the long run, compromises the capability of the whole software and its long-term value.
The price tag is just one aspect of the software; many providers fail to consider costs such as implementation, training, and support. These costs later increase the expense more than the price of the high initial costs. Moreover, many providers buy low-cost software without considering the long-term benefits and ROI.
This makes it difficult to recover the investment, and increasing the revenue is more difficult. The lack of essential features also reduces patient outcomes, further affecting revenue generation. However, the one big mistake in the cost is not asking for the hidden costs, such as upgrade costs, maintenance, and support costs.
So, you need to carefully check all of this, as focusing on affordability can lower the long-term return and revenue generation quite severely.
Failing to Assess Scalability and Customization
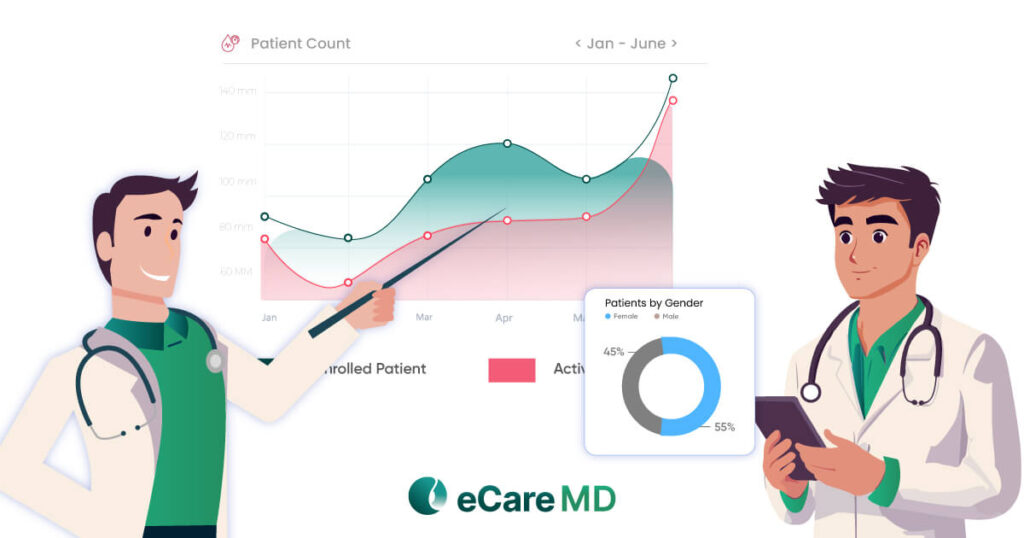
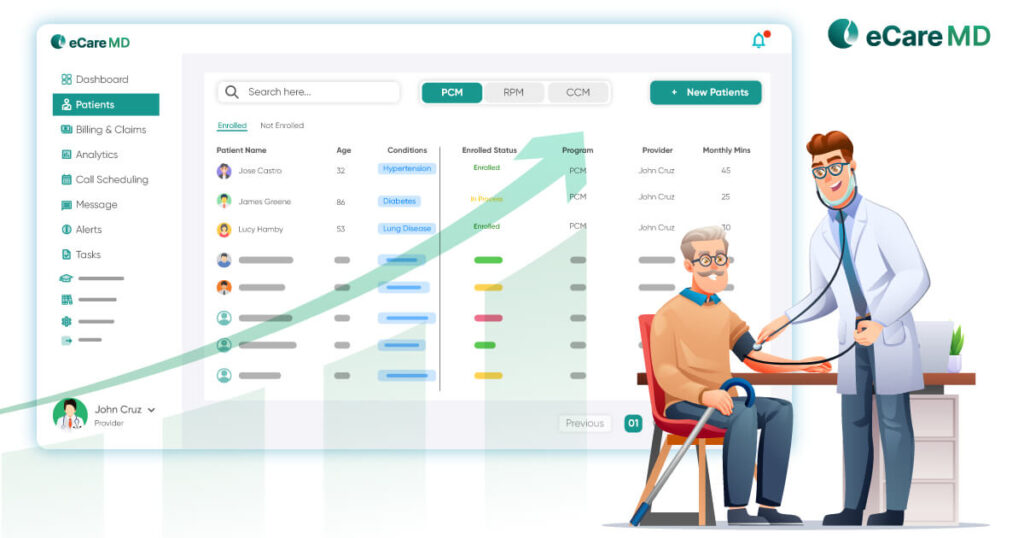
Selecting Principal Care Management (PCM) software isn’t just about meeting your current needs—it’s about ensuring the system can grow with your practice. Many providers make the mistake of choosing software that works for them today but lacks the flexibility to scale as their patient base expands or their care models evolve. If the software can’t accommodate growth, you may find yourself searching for a replacement sooner than expected, leading to unnecessary disruptions and costs.
Customization is another critical factor often overlooked. Every healthcare practice has unique workflows, documentation requirements, and patient engagement strategies. If the PCM software isn’t adaptable to your specific needs, your team may struggle with rigid, inefficient processes that hinder productivity. A platform that allows for workflow customization ensures that your staff can work efficiently without forcing them to conform to a one-size-fits-all system.
Scalability also applies to data management. As your patient volume increases, so does the need for a system that can handle more records, appointments, and care plans without performance issues. Software that isn’t built for high-volume practices may slow down, creating frustrating delays in accessing critical patient information.
Lastly, failing to ask about the vendor’s update and upgrade schedule can leave you stuck with outdated technology. A reliable software provider should have a clear plan for rolling out improvements, addressing security concerns, and integrating new healthcare innovations. Without this, your PCM software could quickly become obsolete, forcing you into yet another costly transition.
Skipping the Vendor's Reputation and Support

When it comes to choosing a vendor, researching their reputation and track record is important. However, many providers skip this step entirely and do not verify the capabilities and experience of the software vendor. Another thing that is most often overlooked is asking for and verifying customer reviews and references.
Knowing the experiences of other healthcare practices can tell you a lot about the vendor’s services and customer support. Apart from this, providers fail to assess the responsiveness of the vendor and later suffer from long downtime during the system failure. Moreover, providers often skip checking the vendor’s track record and case studies to save time. But, this can have severe consequences for the quality of the software, and it may not suit your needs.
Another important aspect that is overlooked is the vendors’ experience with developing the PCM software. Many vendors do not offer PCM software development as their main service but as a side feature. So, verify this before committing, as PCM requirements are different than those of CCM and TCM.
So, you need to avoid these pitfalls to make the best out of PCM software development and implementation. Skipping this step can lead you to software that makes things more difficult and frustrating instead of making them much easier.
Conclusion
There are many common mistakes that providers can make while buying the PCM software, and these mistakes cost the provider extra money. The first mistake to avoid is ignoring the integration capabilities of the software, along with neglecting security and compliance. These mistakes cause a decline in software security and performance by a large percentage.
Moreover, choosing cost over value and failing to assess scalability can cause the return on investment to be lower than the amount invested. So, you need to avoid doing this; apart from this, skipping the verification of vendors’ reputations can affect the quality of the final product.
So, if you want a product that gives long-term value and returns, then contact us, and you will get a tool that will enhance your overall practice and revenue generation.