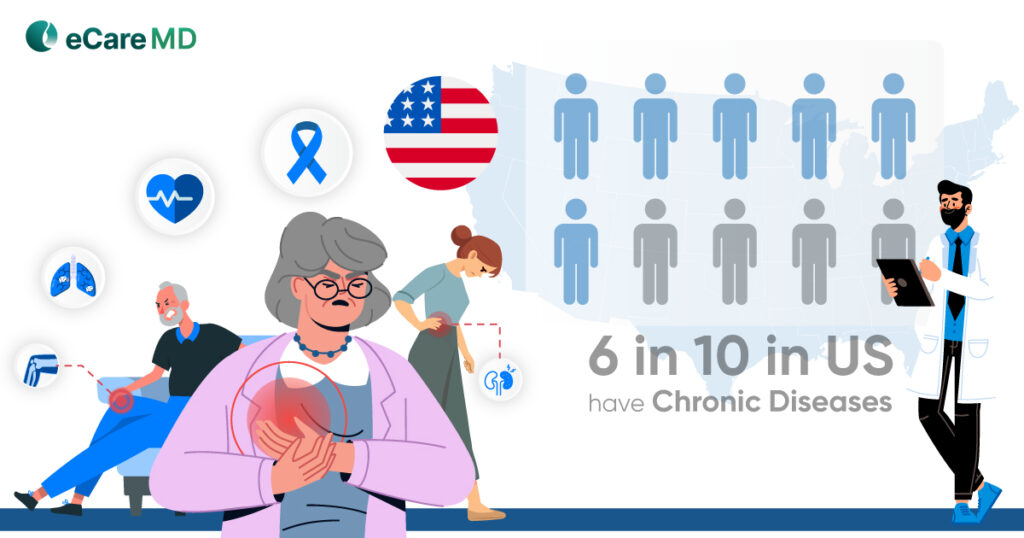
In the US, accounting for chronic disease centers, around 6 Americans out of 10 are fighting with at least one chronic condition, such as asthma, diabetes, depression, and hypertension. Those chronic conditions are life-threatening, expensive, and affecting around 75% of the nation’s expenditure on total healthcare. As we know, patients with chronic conditions require immediate attention and proper treatment to keep patients healthy and stable.
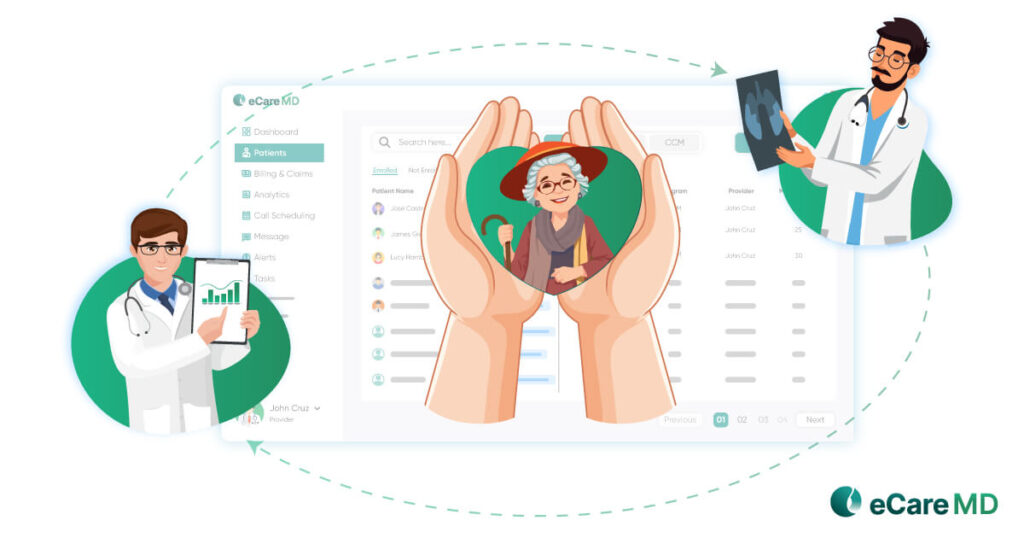
Improved Communication and Collaboration
Consider offering a free downloadable guide on "Optimizing Communication and Collaboration in Patient Care."
Download nowStreamlined Care Transitions
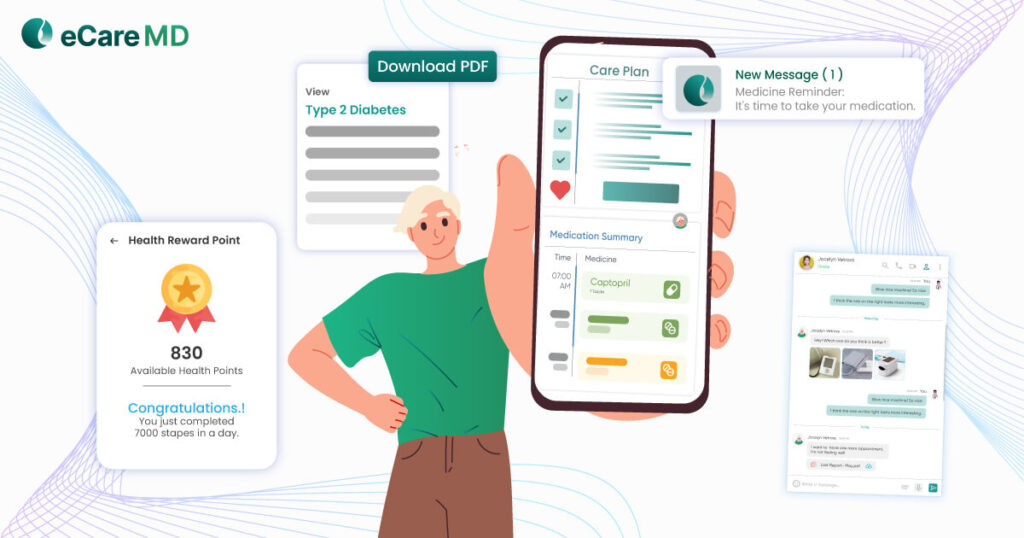
Enhanced Patient Engagement

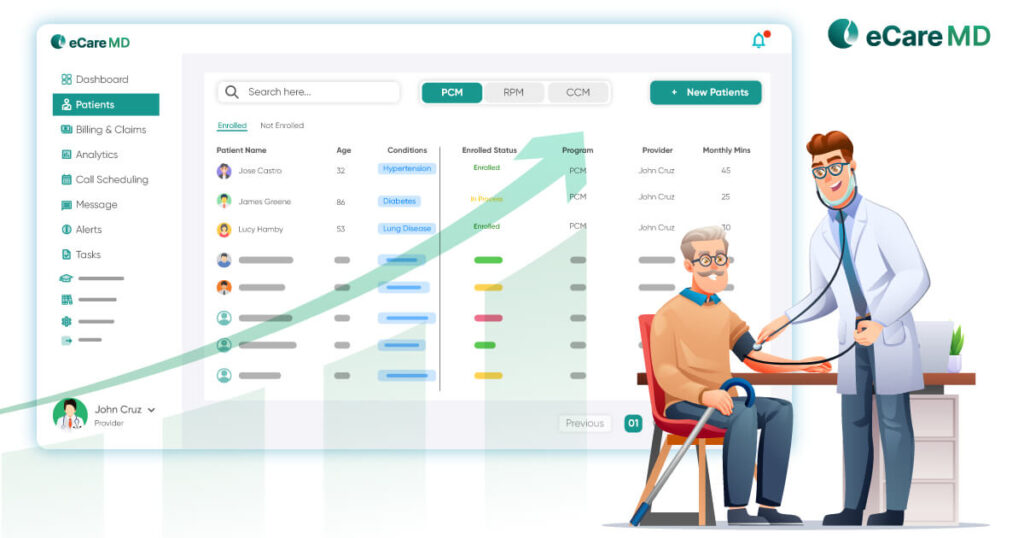
Improved Care Quality and Outcomes
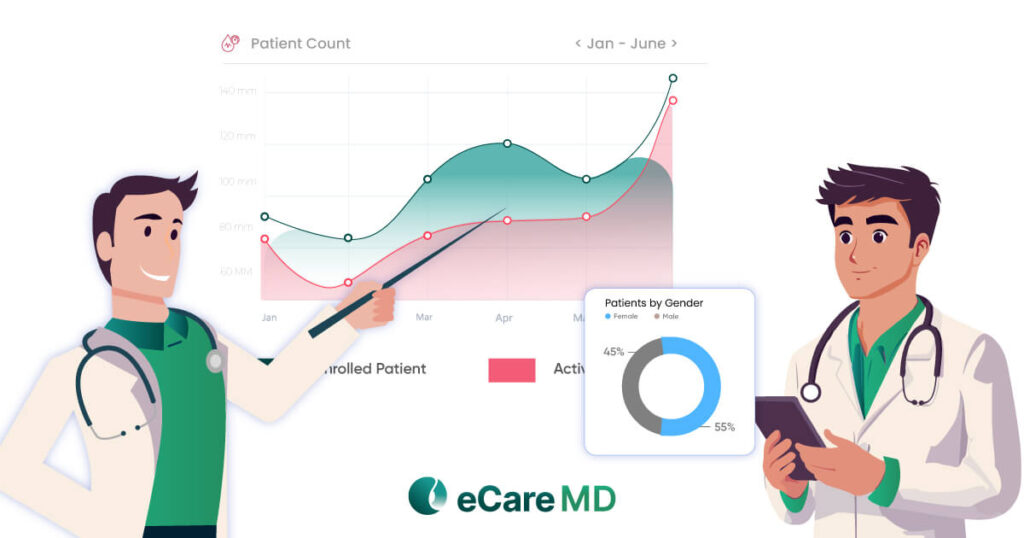
Measure and Improve Performance

Conclusion
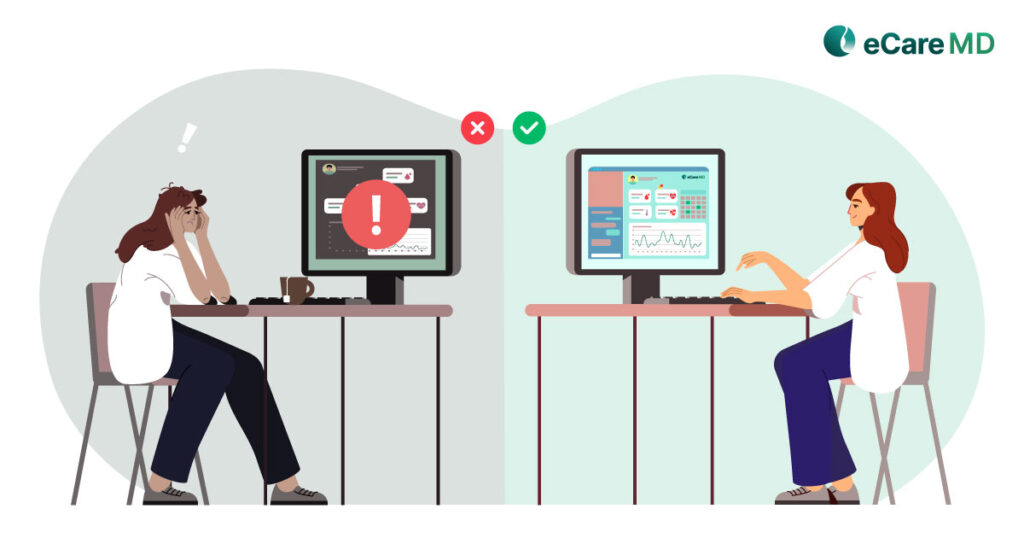
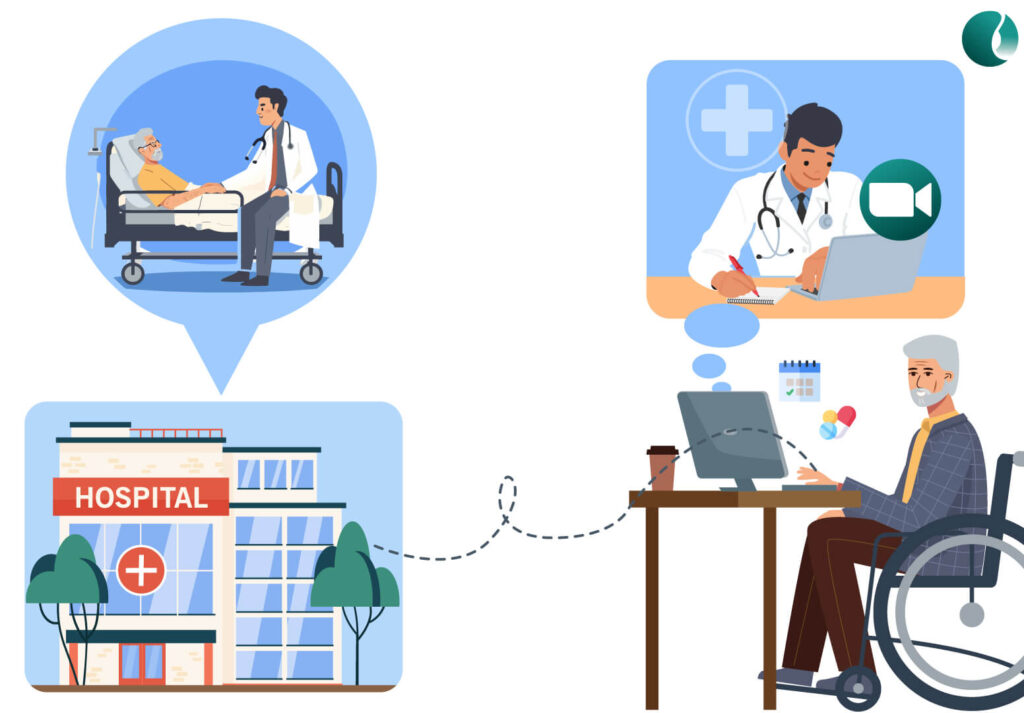
Care coordination software bridges the gap between care providers and patients to ensure smoother and improved patient health outcomes. Many factors help providers improve care coordination, such as technological advancements and functional workflows that ensure seamless care transitions.
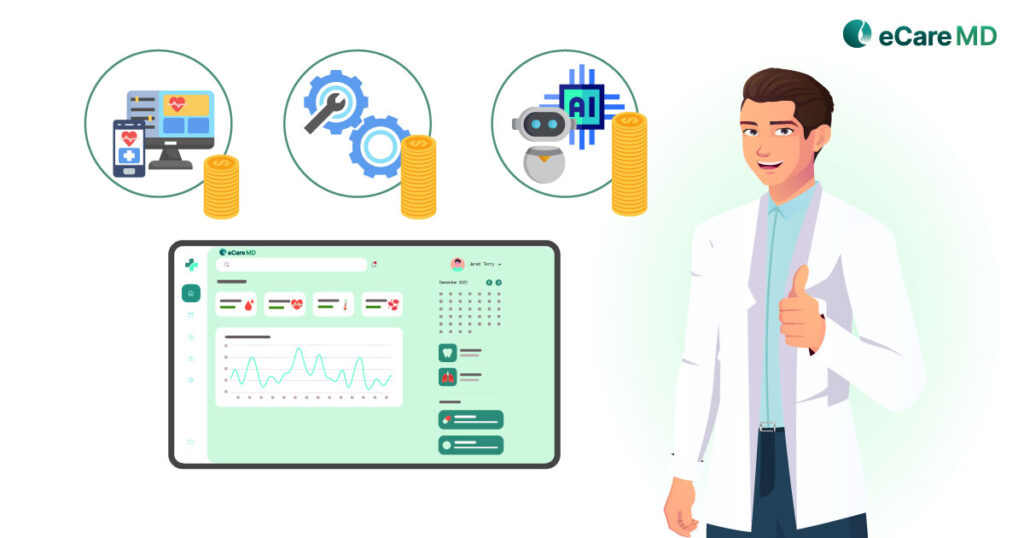
In terms of technology, there are many features that improve patient engagement through telehealth, maintaining medical records, and getting analytics and reporting, which can help healthcare providers get into intervention mode and take any required actions to keep patients safe from any future risk associated with their health.
In terms of functional workflow care coordination software ensures that patients should get the proper and required care in time and quality. Care coordination software helps providers to set their SOP to treat patients and by following those they can achieve better patient outcome.
Hence By fostering a symphony of care, not a cacophony of services, care coordination software empowers providers to deliver the high-quality, patient-centered care we all strive for.
Frequently Asked Question’s
There are multiple benefits of implementing care coordination software at healthcare practices explained into three main categories below:
Improved care coordination
- Acts as a bridge for patient care- Acts as a center of care, allowing all providers to access patient health information and the ability to visualize and take any necessary actions by collaborating with other providers and patients.
- Better care plan and review- Streamlined communication leads to improved care plan adherence and addressing of patient needs inline with care plan goals and requirements.
- Enhanced task management- Micro Level task management is the key to care coordination software, which enables all healthcare professionals to schedule and complete the tasks that are associated with patient health, which ensures timely healthcare delivery.
Enhanced Efficiency and Cost Savings:
- Streamlined Workflows- Automating tasks like sending out referrals and accepting the outside referrals and appointment reminders through email and text frees up time for providers to focus on patient care.
- Reduced Readmissions- Improved care coordination by early detection of health risks and real-time interventions can lead to fewer complications and hospital readmissions, saving healthcare costs.
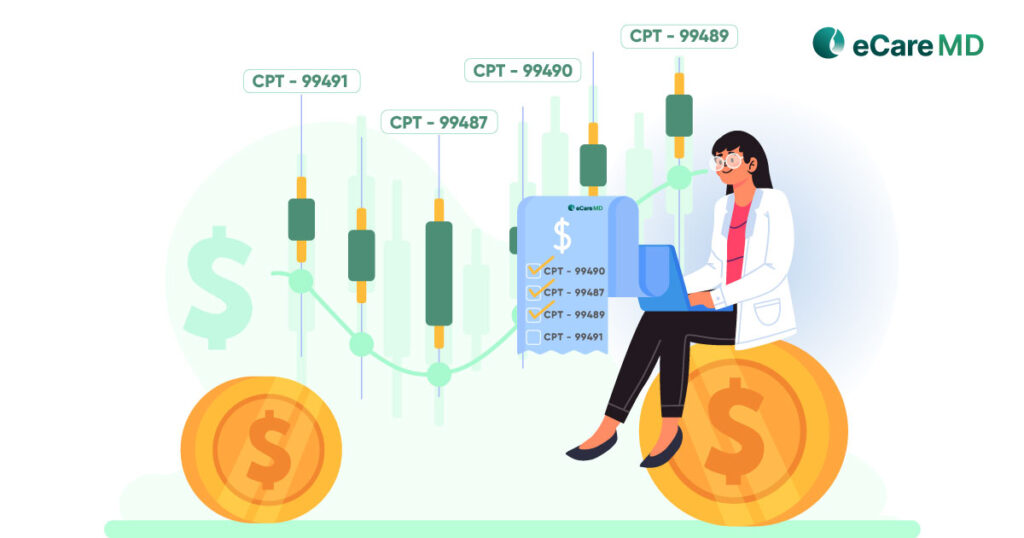
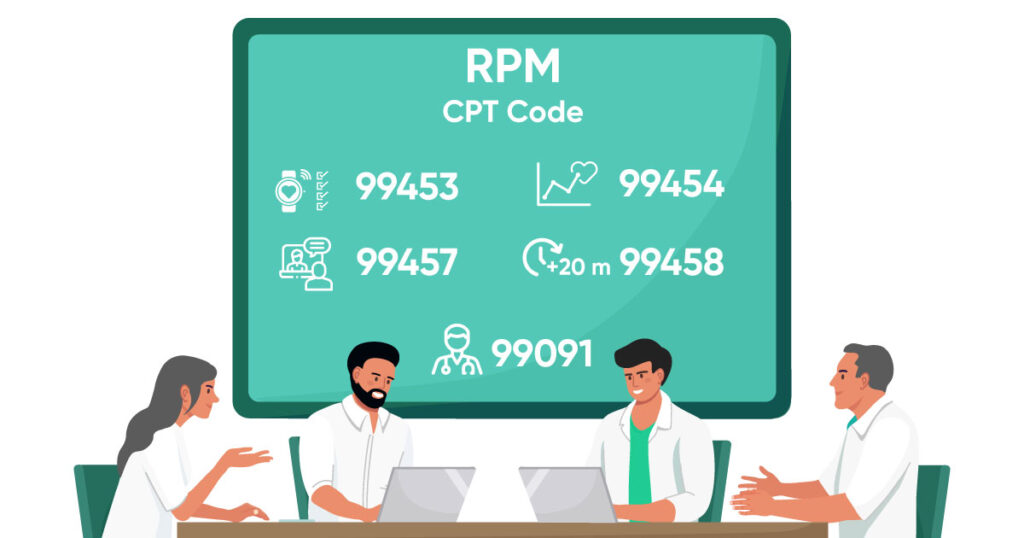
- Accurate Billing- Automated time tracking along with the services provided to patients, as well as care coordination software, can help ensure accurate and complete billing, maximizing reimbursement for practices.
Improved Patient Outcomes:
- Increased Engagement- Patient engagement is the major part of the care coordination platform, and it can be achieved with telehealth features such as secure text messaging and audio/video calling. Patients can access information and schedule appointments more easily, fostering better engagement in their care.
- Reduced Errors- Clear communication and centralized data minimize the risk of errors in medication or treatment plans.
- Improved Quality of Care- By ensuring everyone is on the same page, care coordination software contributes to a higher quality of care for patients.
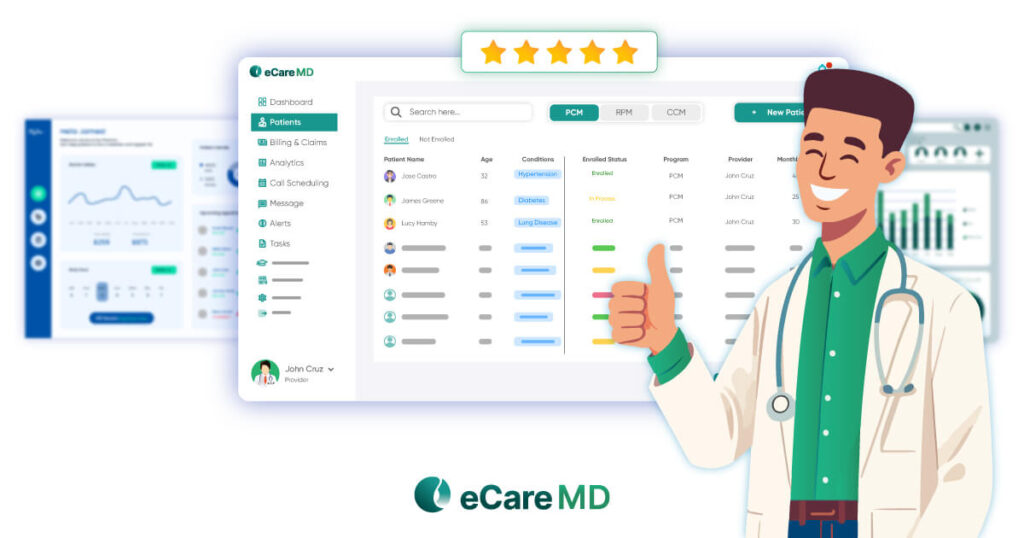
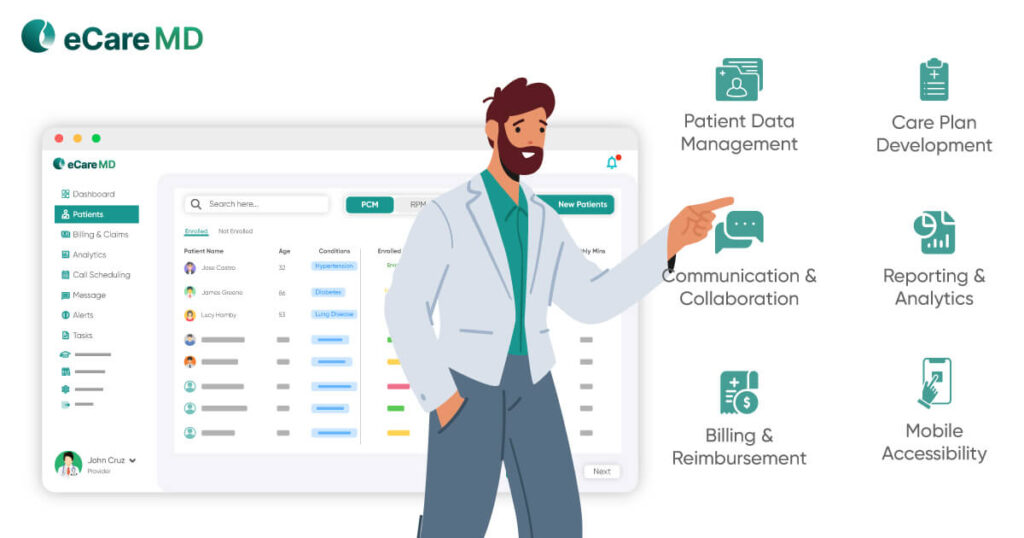
The care coordination platform provides a wide range of features that help providers access patient health information at their fingertips. Also, robust reporting and analytics give health insight that can be used for assessing patient health conditions and identifying any future complications and risks associated with patient health. To overcome those risks and complications, care coordination software has multiple engagement options through which they can connect with patients and ensure patients keep away from health risks by taking appropriate actions.
Additionally, creating fostered care plans, help patients to keep adhere to assigned care plans, timely review and intervene as and when required helps providers to achieve enhanced patient outcomes.
In order to deliver quality care, healthcare providers should have an appropriate care coordination platform which consists of all features, security measures and compliance with all regulatory requirements.
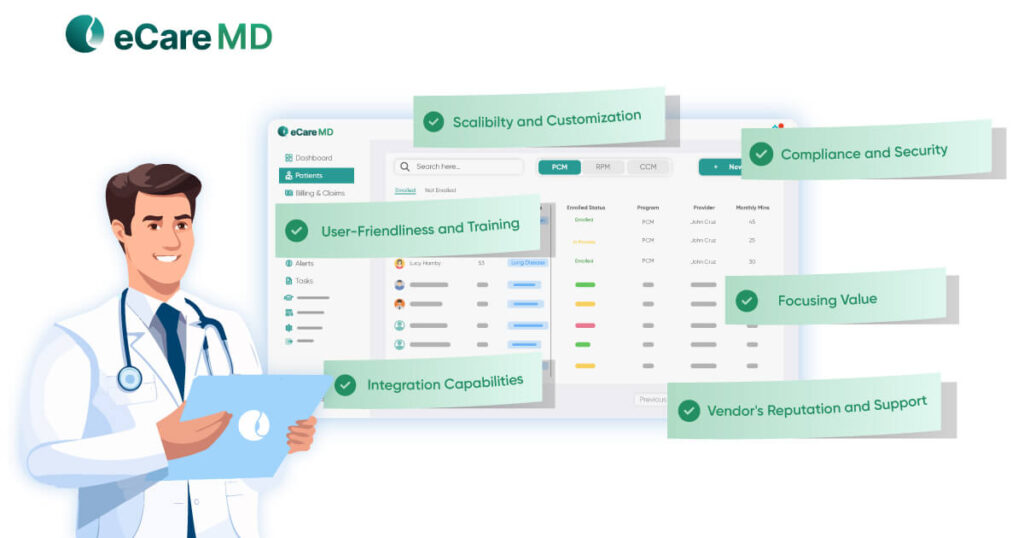
Below are some factors that should be considered while selecting a care coordination platform:
- Care coordination Platform should have supporting features like care plan creation and secure messaging, integrating smoothly with EHR systems, and providing crucial analytics for tracking KPIs.
- A platform’s usability and user-friendly interface boosts adoption among healthcare staff. Essential security features include HIPAA compliance to protect patient data. Additionally, scalability is crucial, allowing the platform to grow with your needs.
- When assessing usability and security, it’s important to evaluate the software provider’s support for implementation and training. Additionally, compare pricing models to ensure affordability and research the vendor’s reputation and customer support history to gauge reliability.
Healthcare providers can effectively implement care coordination initiatives by adopting a comprehensive strategy that includes
- Integrating advanced health information systems for real-time data sharing
- Enhancing staff training on care coordination principles,
- Fostering open communication across all team members.
- Establishing clear protocols and continuous evaluation mechanisms,
- Along with building collaborative partnerships across healthcare disciplines and community resources,
These are the main parameters for improving patient outcomes and increasing system efficiency.
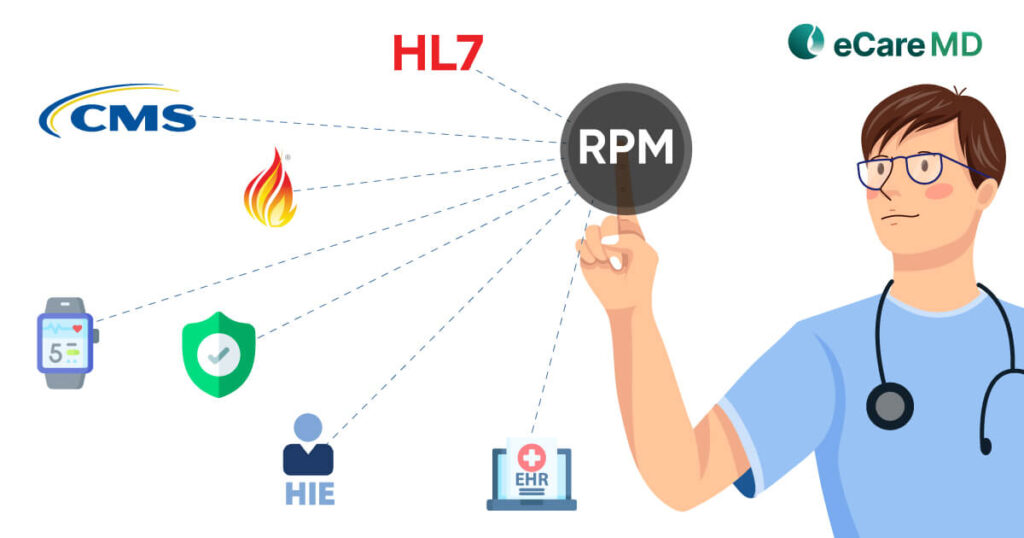
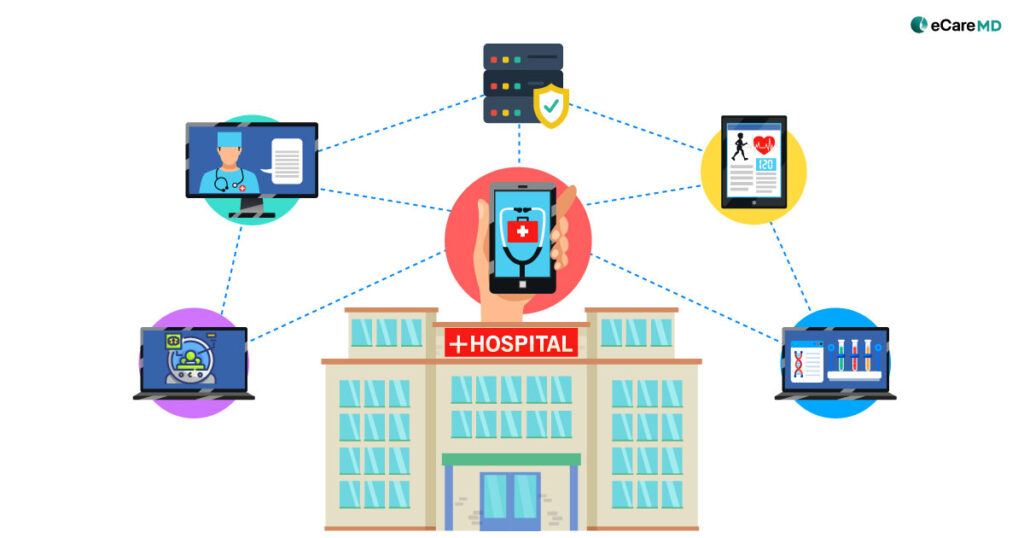
Interoperability plays an important role in enhanced care coordination by making seamless data exchange between multiple healthcare digital platforms and software. This integration enables healthcare providers to access and share patient health records in real time to make critical, informed health decisions by providing quality patient care.
Interoperability enhances the accuracy of diagnoses, streamlines treatment processes, and reduces the likelihood of errors, thereby improving overall patient outcomes and operational efficiency within healthcare organizations.
While adopting the care coordination software, some required security and privacy measures need to be taken into account. Below are some example
- Data Encryption- While implementing care coordination software providers should ensure that all data transmitted and stored within the software should be encrypted and protected.
- Role-based access control- Implementing role-based access control ensures that only authorized personnel can access sensitive patient health data, which restricts the chances of data breaches.
- Audit Trails- Audit trails that log all access and actions taken by users, providing an accountability mechanism to monitor and review usage and potential security incidents.
- Compliance with Regulations- The software must have compiled with required healthcare regulations and standards such as HIPAA (Health Insurance Portability and Accountability Act) in the U.S.
- Data Integrity and Backup- Ensure mechanisms are in place for data integrity checks and regular backups to protect data from loss or corruption and to allow for recovery in case of an incident.